First branchial cleft anomaly
By Thomas AK, Jorgensen SA, Towbin AJ, Towbin R
CASE SUMMARY
A 6-year-old girl presented with localized swelling and redness located anterior and inferior to her right ear. There is a history of intermittent swelling in this region with fever and purulent drainage from the ear.
IMAGING FINDINGS
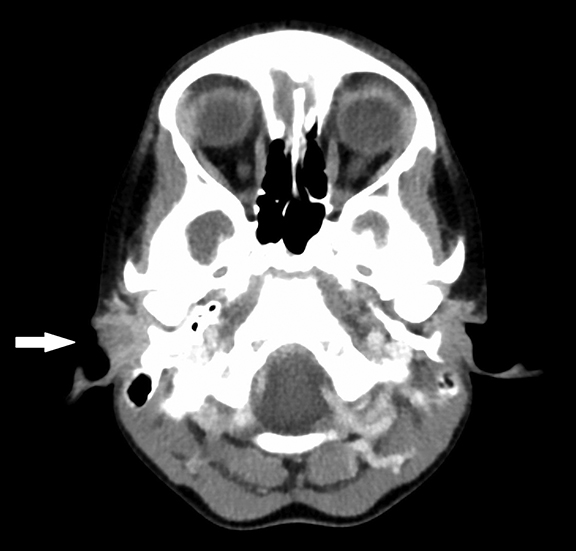
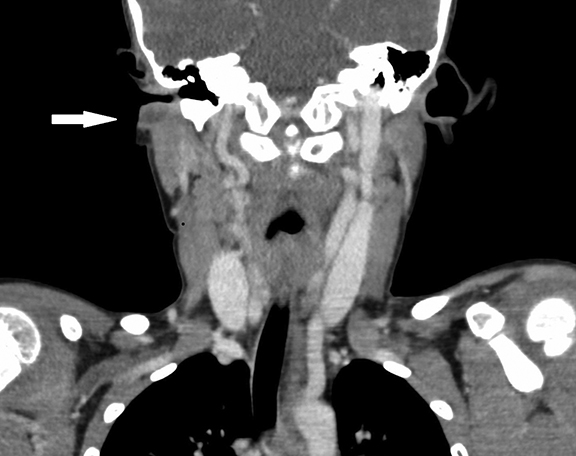
Axial (Figure 1A) and coronal (Figure 1B) images from a CT examination of the neck with IV contrast show a complex, rim-enhancing lesion in the right parotid region, just inferior to the right external auditory canal.
DIAGNOSIS
First branchial cleft anomaly.
Differential diagnoses include: suppurative abscess, benign lymphoepithelial cyst, venolymphatic malformation, and nontuberculous mycobacterial adenitis.
DISCUSSION
First branchial cleft anomalies are a special group of congenital head and neck malformations. These lesions are rare, accounting for 8% of all branchial cleft anomalies.1 They are typically located in the anatomic Pochet’s triangle.2 The margins of Pochet’s triangle are the external auditory canal superiorly, the mental region anteriorly, and the hyoid bone inferiorly.2
There are 6 pairs of branchial arches, which appear around the 4th week of gestation. These arch pairs are separated by 5 clefts externally and 5 pouches internally.1 The branchial arches fuse and the clefts are obliterated by the 7th week of development. The cavum conchae, the external auditory canal (EAC) and the external layer of the tympanic membrane are the structures derived from the first branchial cleft.3 First branchial cleft lesions result from incomplete fusion of the ventral portions of the first and second arches.3 First branchial cleft anomalies are associated with the parotid gland, as closure of the branchial clefts is concurrent with the emergence of the developing parotid gland and migration of the facial nerve, which originate from the second branchial arch.1 First branchial cleft malformation develops more often near the ear and parotid gland than the hyoid region.
Several classification systems have been proposed for first branchial cleft anomalies. The first system, proposed by Arnot in 1971, categorized anomalies into 2 types.4 Type 1 anomalies involve the parotid region and manifest during early or middle adult life.4 Type 2 anomalies occur during childhood and arise in the anterior cervical triangle with a communicating tract to the external auditory canal.4 Work proposed the second classification system in 1972. This is the most widely used classification system today. Work’s system uses a 2-part histologic classification of these anomalies.5 Work type 1 anomaly is a defect of ectodermal origin, arising from the duplication of the membranous EAC.5 A Work type 2 anomaly is ectodermal and mesodermal in origin, arising from duplication of the membranous external auditory canal, cartilaginous pinna, and rarely from the second branchial arch.5 The third classification system was proposed by Olsen et al. in 1980; that system classifies anomalies into cysts, sinuses or fistulas.6
The most common presentation of patients with branchial cleft anomalies is swelling in the cervical (35%), parotid (35%) or periauriclar (24%) regions. Anomalies frequently become infected. An inflammatory process in the region of Pochet’s triangle should immediately raise suspicion for this anomaly. Otorrhea is a common symptom. This anomaly should be suspected if recurrent or chronic otorrhea is present in the absence of chronic otitis. A sinus or fistula opening in the external auditory canal is present in only 44% of patients, and may be difficult to find even when present.2
CONCLUSION
First branchial cleft malformations are often under recognized and mistaken for other inflammatory lesions in the periauricular and cervical region. Complete removal is needed to prevent recurrence or secondary infection; therefore delay in recognition can lead to complications. This entity should be considered in all patients with chronic, unexplained otorrhea or recurrent parotid space abscess.
REFERENCES
- Koeller K, Alamo L, Adair C, et al. Congenital cystic masses of the neck: Radiologic-pathologic correlation. Radiographics. 1999;19:121-146.
- Sichel J, Halperin D, Dano I et al. Clinical update on type II first branchial cleft cysts. Laryngoscope.1998;108:1524–1527
- Benson M, Dalen K, Mancuso A et al. Congenital anomalies of the branchial apparatus: Embryology and pathologic anatomy. Radiographics. 1992;12:943–960.
- Arnot R. Defects of the first branchial cleft. South African Journal of Surgery.1971;9:93-98.
- Work W. Newer concepts of first branchial cleft defects. Laryngoscope. 1972; 82:1581-1593.
- Olsen K, Maragos N, Weiland L. First branchial cleft anomalies. Laryngoscope. 1980; 90:423-436.
- Triglia J, Nicollas R, Ducroz V et al. First branchial cleft anomalies: A study of 39 cases and a review of the literature. Arch. Otolargyngol. 1998;124:291-295.
