Perforated Meckel Diverticulum
Images
Case Summary
A teenager presented with a one-day history of non-bloody, non-bilious emesis, incomplete defecation, and periumbilical abdominal pain with an episode of extreme groin and anal pain. The patient had a medical history significant for a right inguinal hernia repair. While vital signs were normal, laboratory evaluation revealed a markedly elevated white blood cell count of 21,850/mm3 with a left shift.
Imaging Findings
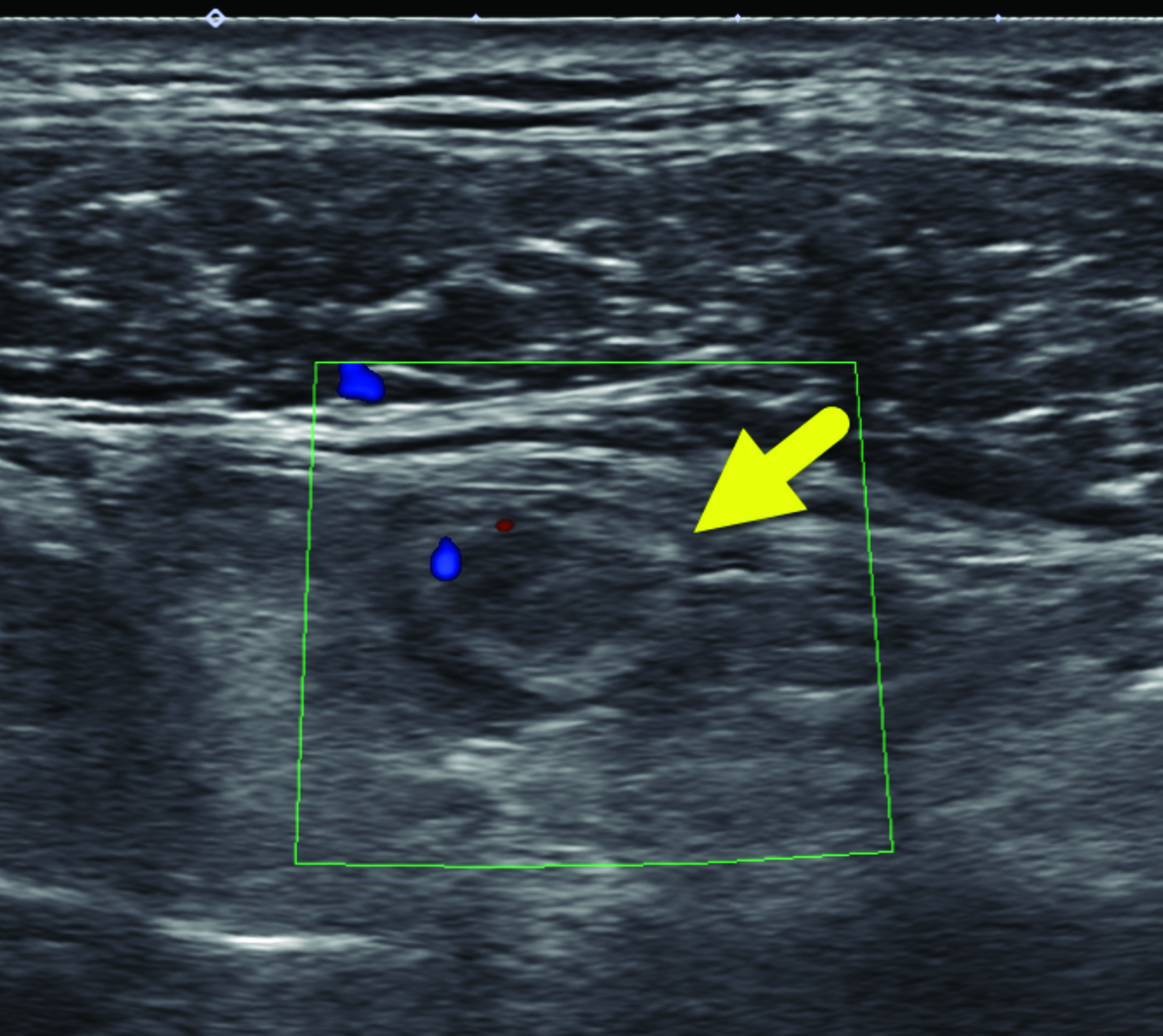
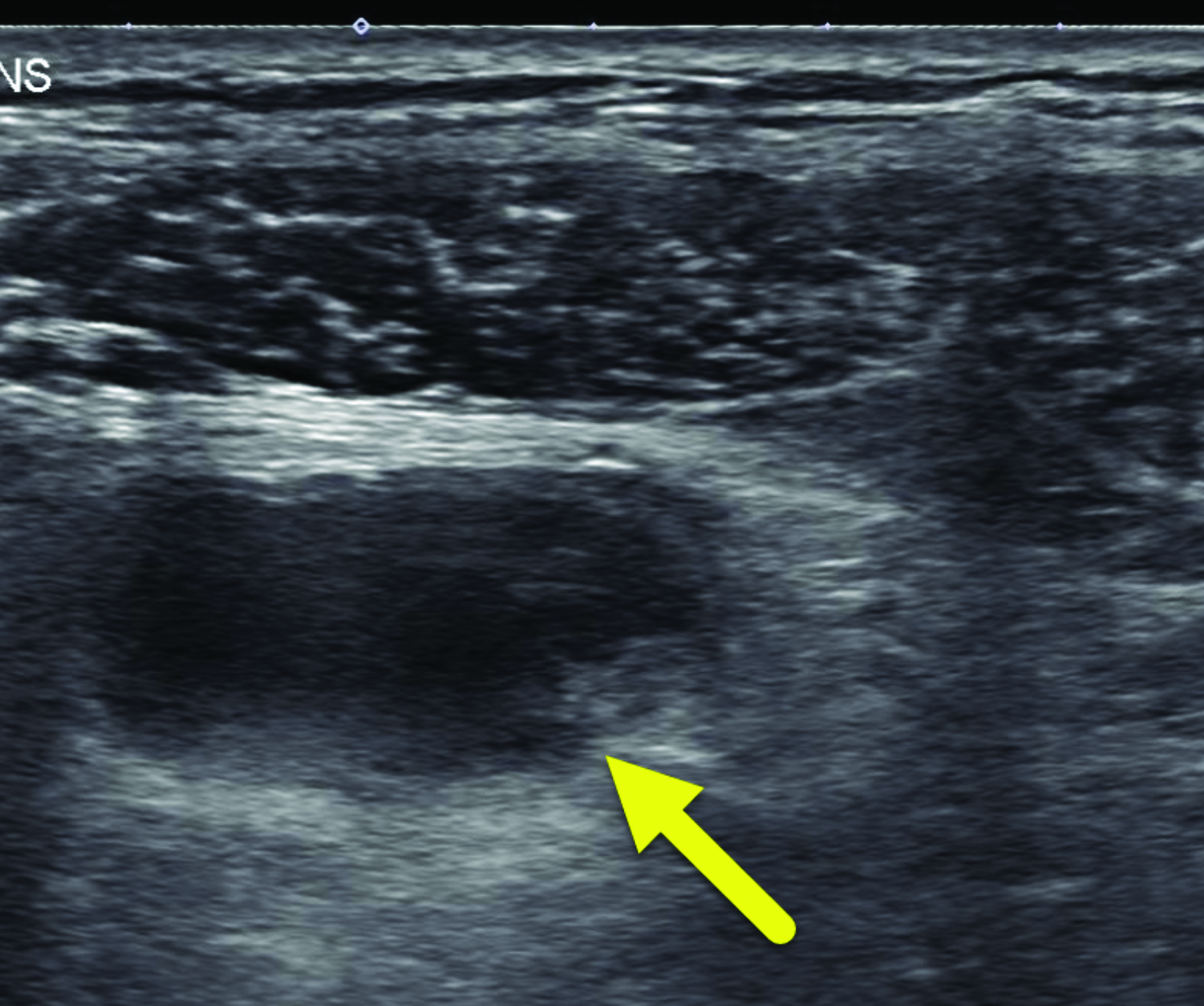
A right lower quadrant ultrasound (Figure 1) was performed to evaluate for appendicitis. The scan did not show the appendix. However, a tubular structure was visible that did not connect to the cecum. The tubular structure had a thickened wall, associated echogenic fat, and mild wall hyperemia. A small collection with internal debris was visible adjacent to the tubular structure.
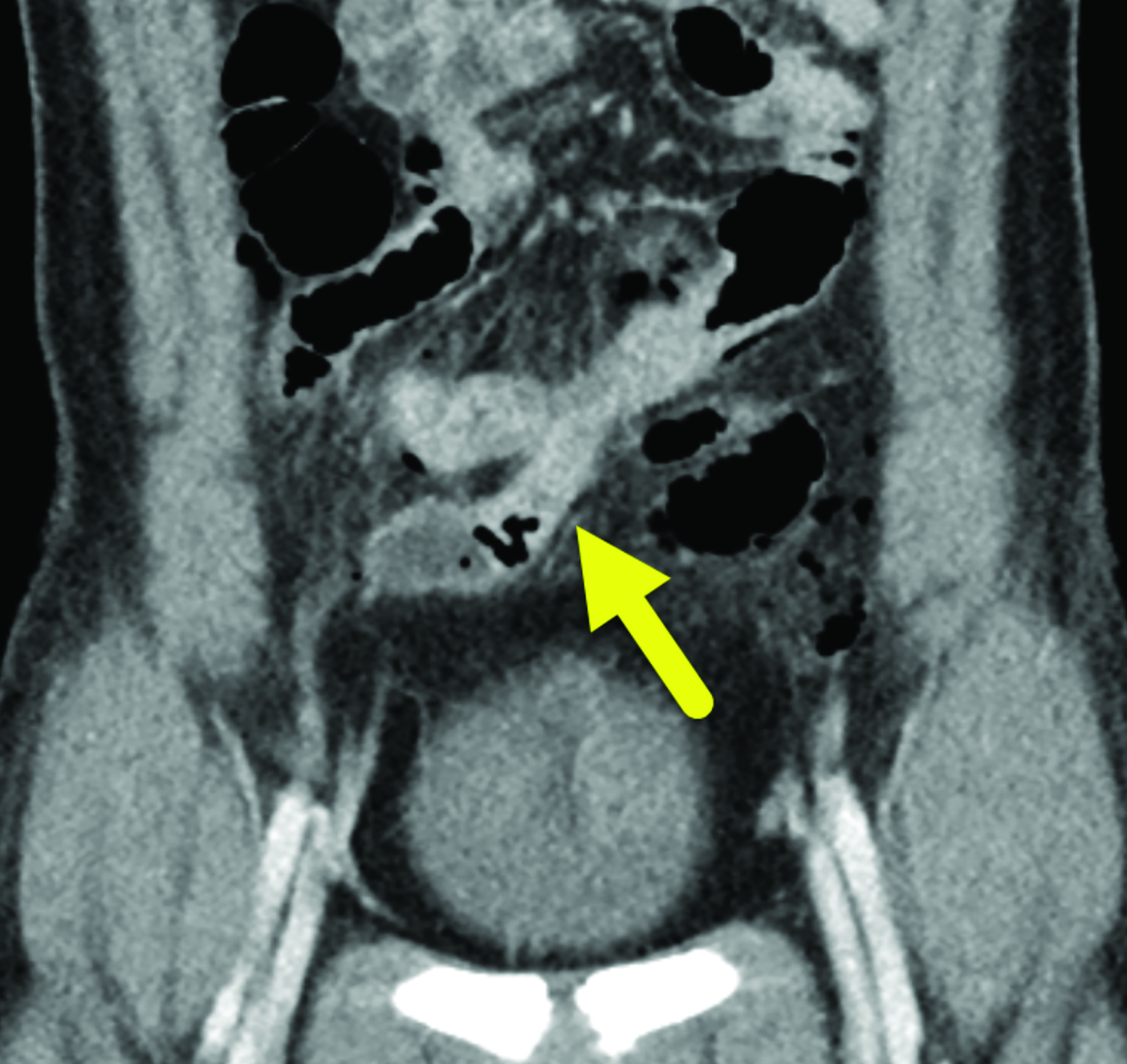
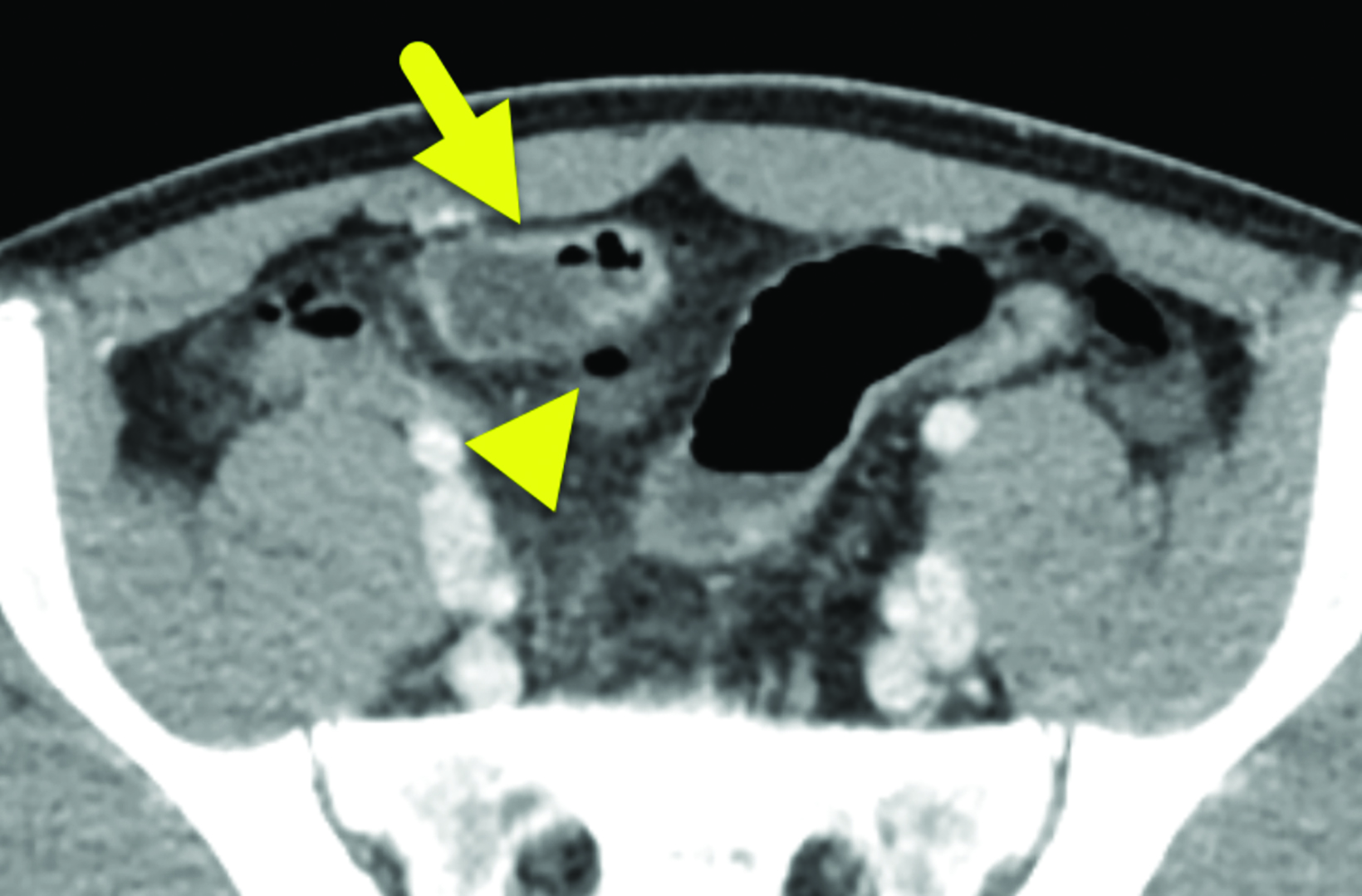
The study was interpreted as indeterminate for appendicitis. A computed tomography (CT) scan (Figure 2) showed a dilated, blind-ending tubular structure measuring up to 2.1 cm in diameter in the mid-lower abdomen. This appeared to arise off the antimesenteric side of the distal ileum, with hyperenhancement of the mucosa. There was some irregularity and discontinuity along the posterior aspect of the structure with scattered areas of free air within the peritoneal cavity. An additional, non-enhancing fluid collection was seen in the retrovesicular pouch. The appendix was identified and appeared normal.
Surgical pathology revealed a perforated ileum at the junction with a Meckel diverticulum containing ectopic gastric mucosa.
Diagnosis
Ruptured Meckel diverticulum
Discussion
A Meckel diverticulum is a congenital anomaly of the gastrointestinal tract, occurring in 0.3-2.9% of the population.1 It results from incomplete regression of the vitelline duct during the 10th through 12th weeks of gestation. The result is a blind pouch at the antimesenteric border of the terminal ileum, with variable location up to 200 cm proximal to the ileocecal valve.1 There are other anomalies of the vitelline duct, including an umbilical sinus or ileo-intestinal fistula; however, these account for only 2% of vitelline duct abnormalities. Pathologically, a Meckel diverticulum is expected to contain normal intestinal mucosa. However, ectopic tissue is common; it most frequently arises from the stomach or pancreas.2
A Meckel diverticulum can become symptomatic for one of two reasons: obstruction causing diverticulitis, or the effects of ectopic tissue. Patients with symptomatic Meckel diverticulitis classically present with abdominal pain and are often misdiagnosed with appendicitis. Patients with ectopic gastric mucosa may first present with painless gastrointestinal bleeding.
Although it occurs with similar frequency in males and females, Meckel diverticulum is more commonly symptomatic in males.3 The causes for symptomatic Meckel diverticulum are not limited to the inflammation seen in Meckel diverticulitis. A systematic review of the etiology of symptomatic Meckel diverticula showed that approximately 47% of cases in children present with obstruction (a large portion resulting from intussusception), 25% of cases with painless gastrointestinal bleeding, and 20% with inflammation.1,2
Other complications of a Meckel diverticulum include perforation, neoplasm, and enterolith formation.4 In most patients, a Meckel diverticulum-associated complication is not the initial diagnosis, and these cases are often misdiagnosed as appendicitis, colonic diverticulitis, other bowel obstruction, or endometriosis.5
Imaging plays a key role in early diagnosis of Meckel diverticulum and its associated complications. Ultrasonography is often first-line imaging in patients presenting with abdominal pain. On right lower-quadrant ultrasound, a diverticulum will have the appearance of normal gut. The tubular, blind-ending pouch will appear continuous with the ileum and often be mistaken for the appendix. Identifying the normal appendix can
help the radiologist make a more confident diagnosis of Meckel diverticulitis.
The diverticulum may be difficult to visualize on CT, but it appears as a blind-ending structure of small bowel proximal to the ileocecal valve.6 When it is inflamed, CT shows increased mural thickness along with signs of mesenteric inflammation. Bowel obstruction caused by a diverticulum can be visible with the presence of a transition point, volvulus, or intussusception. A small-bowel perforation should be suspected when free intraperitoneal air is present.7
Gastrointestinal bleeding is often caused by ectopic gastric mucosa. In these instances, scintigraphy with99mTc-pertechnetate has an 85-90% sensitivity in the pediatric population.8 The radiologist should look for fixed accumulation of the radiopharmaceutical that becomes visible at the same time gastric mucosa is visible.
Conclusion
Meckel diverticulum is a congenital abnormality that occurs in up to 3% of the population. Accurately diagnosing its complications remains a challenge. Diagnostic imaging plays a key role in the work-up of patients with abdominal pain or painless gastrointestinal bleeding.
References
- Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel’s diverticulum in the 21st century. Medicine (Baltimore). 2018;97(35):e12154. doi:10.1097/MD.0000000000012154.
- Huang CC, Lai MW, Hwang FM, et al. Diverse presentations in pediatric Meckel’s diverticulum: a review of 100 cases. Pediatr Neonatol. 2014; 55(5):369-375. doi: 10.1016/j. pedneo.2013.12.005. Epub 2014 Mar 28. PMID: 24685339.
- Levy AD, Hobbs CM. From the archives of the AFIP. Meckel diverticulum: radiologic features with pathologic correlation. Radiographics. 2004; 24(2):565-587. doi: 10.1148/ rg.242035187. PMID: 15026601.
- Choi SY, Hong SS, Park HJ, Lee HK, Shin HC, Choi GC. The many faces of Meckel’s diverticulum and its complications. J Med Imaging Radiat Oncol. 2017; 61(2):225-231. doi: 10.1111/1754-9485.12505. Epub 2016 Aug 4. PMID: 27492813.
- Francis A, Kantarovich D, Khoshnam N, Alazraki AL, Patel B, Shehata BM. Pediatric Meckel’s diverticulum: Report of 208 cases and review of the literature. Fetal Pediatr Pathol. 2016; 35(3):199-206. doi: 10.3109/15513815.2016.1161684. Epub 2016 Apr 11. PMID: 27064958.
- Kotha VK, Khandelwal A, Saboo SS, et al. Radiologist’s perspective for the Meckel’s diverticulum and its complications. Br J Radiol. 2014;87(1037):20130743. doi:10.1259/bjr.20130743.
- Elsayes KM, Menias CO, Harvin HJ, Francis IR. Imaging manifestations of Meckel’s diverticulum. AJR Am J Roentgenol. 2007; 189(1):81-88. doi: 10.2214/AJR.06.1257. PMID: 17579156.
- Poulsen KA, Qvist N. Sodium pertechnetate scintigraphy in detection of Meckel’s diverticulum: is it usable? Eur J Pediatr Surg. 2000; 10(4):228-31. doi: 10.1055/s-2008-1072364. PMID: 11034511.
References
Citation
AA M, MA M, RB T, Y L, CM S, AJ T. Perforated Meckel Diverticulum. Appl Radiol. 2022;(3):53-55.
April 26, 2022