Primary intracranial extraskeletal chondrosarcoma
Images

CASE SUMMARY
A 40-year-old female who had a transient ischemic attack-like “spell” one Saturday sought medical attention the following Monday from her personal physician, who ordered a head MRI and a carotid ultrasound. Presumably, no CT scan of the head was obtained because she was asymptomatic at that point, and such an exam would have yielded little useful information. The MRI scan revealed a mass; upon consultation with the neurology team, it was believed that the mass was probably a meningioma, and that the patient’s spell was likely a seizure caused by the mass. The options given to the patient were surgery or observation, and she decided to proceed with surgery.
During surgery, the mass was found to be of unusual consistency for a meningioma. Gross total resection of the mass was performed, with the origin confirmed to be at the tentorial notch. Follow-up imaging has since demonstrated no evidence of recurrence or residual tumor as of this report.
IMAGING FINDINGS
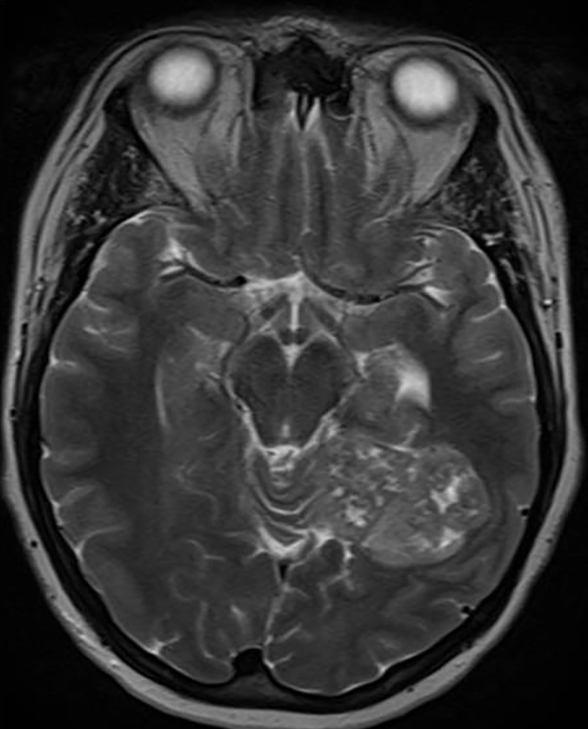
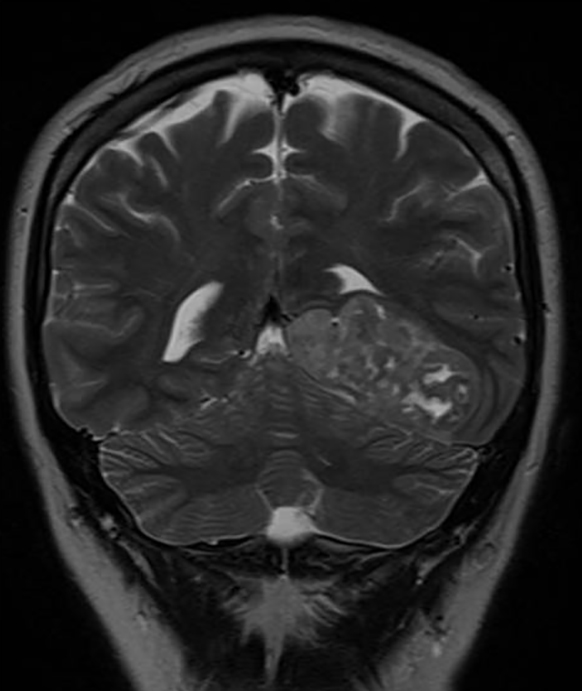
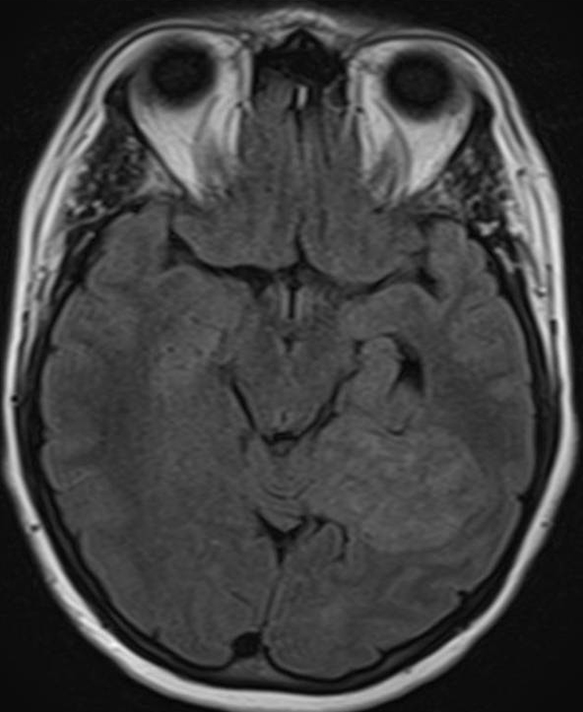
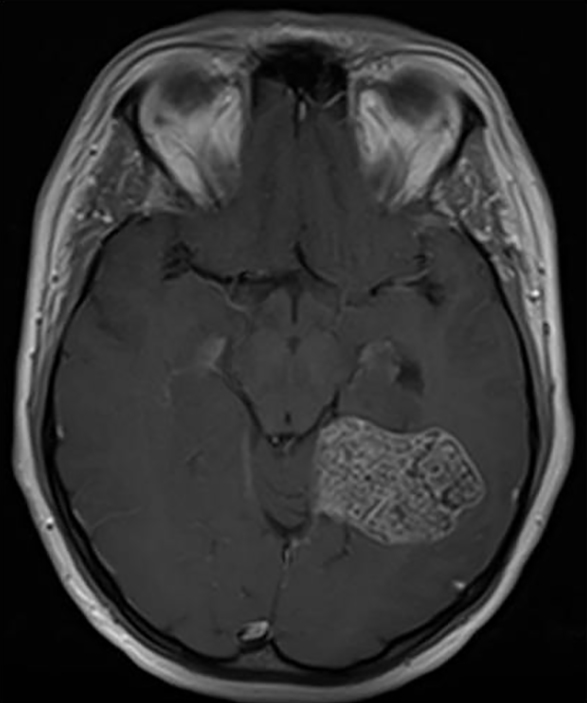
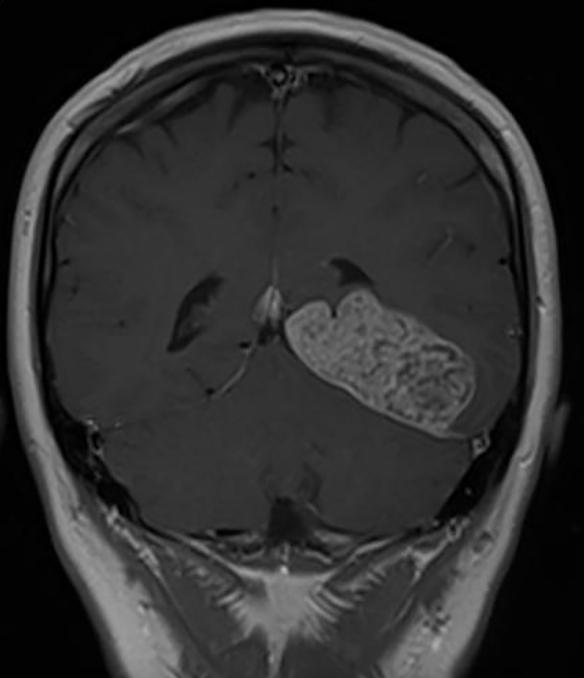
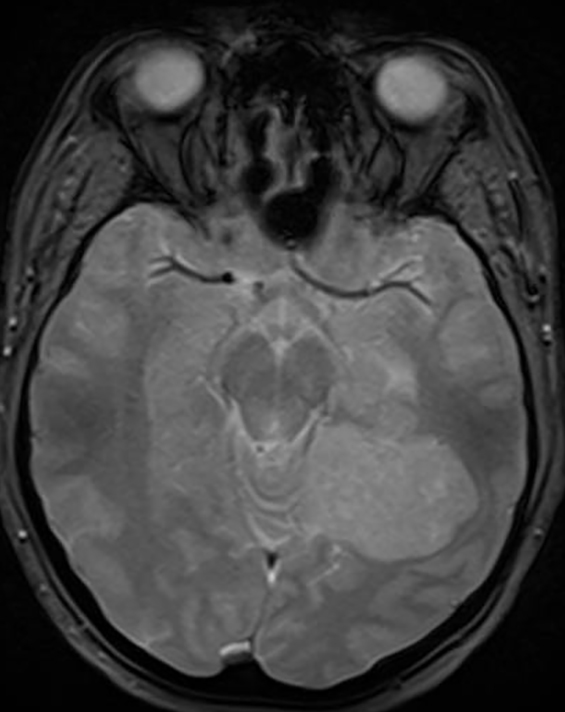
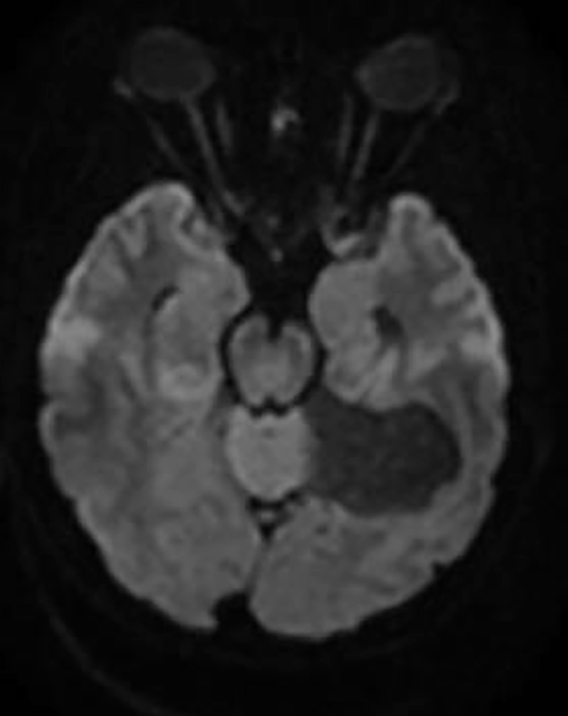
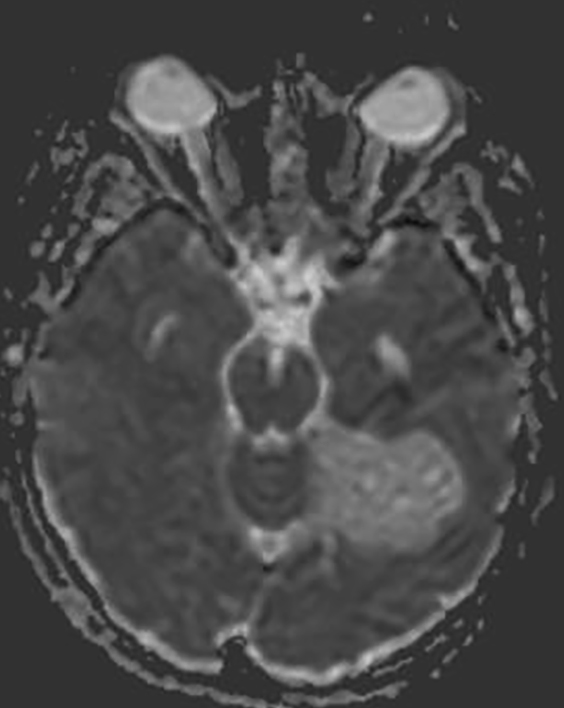
The MRI revealed a low T1 and heterogeneous T2 signal extra-axial, enhancing lesion along the left tentorium cerebelli, with no edema in the adjacent brain parenchyma. No foci of low signal were seen on the susceptibility-weighted images to suggest calcification, and there were no areas of restricted diffusion (Figures 1-5).
DIAGNOSIS
Pathology review was consistent with a low-grade chondrosarcoma, either primary or metastatic. A postoperative CT scan of the chest, abdomen, and pelvis was negative for malignancy; therefore, the final diagnosis was primary intracranial extraskeletal chondrosarcoma. The differential for an extra-axial enhancing lesion on MRI includes meningioma, hemangiopericytoma, and metastasis.
DISCUSSION
Chondrosarcomas are typically seen in the long bones, but they can rarely be seen as primary tumors of the central nervous system.1 When found in the central nervous system, approximately 75% of chondrosarcomas arise from the skull base, but they can also arise from the dura mater, choroid plexus, or the brain parenchyma.1-3 Primary intracranial chondrosarcomas represent less than 0.16% of all primary intracranial lesions.1,4
Extraskeletal cartilaginous tumors are divided into two groups: those associated with the central nervous system and those associated with soft tissue or muscle.4,5 Primary cartilaginous tumors of the CNS usually present as solitary lesions. Most cases occur at the skull base, but can be seen in other locations, including the dura mater, which is extremely rare, but demonstrated by our case.1-3,6,7 They can also be associated with Ollier disease and Maffucci syndrome.1,7
The exact histogenesis of extraskeletal cartilaginous tumors is obscure, with three leading hypotheses presented in literature. These tumors may result from metaplasia of fibroblasts, be derived from primitive mesenchymal cells, or possibly arise from embryonal rests of the cartilaginous matrix within the bone.2,5,6
Three histologic variants have been reported: mesenchymal, myxoid, and classical. The mesenchymal variant is the most common, while the classical variant is extremely rare.6 In a series performed by Korten et al, there was no clear demographic pattern.2 However, within the variants, the mesenchymal variant tends to occur between 20 and 30 years of age, with a slight female predominance.1,4 Furthermore, the classical variant tends to occur between 60 to 70 years of age.1,8 From a prognostic standpoint, the mesenchymal variant tends to behave more aggressively, often with frequent local recurrences shortly after initial treatment, or with metastatic disease.5,9
The imaging findings are nonspecific, and can represent other neoplasms, particularly metastases if the patient has a known primary neoplasm elsewhere. If dural based, the differential includes meningioma and hemangiopericytoma. If intra-axial, a vascular malformation should be considered. Careful attention to the images with observation of a few key findings can raise the suspicion for an intracranial chondrosarcoma. Extra-axial lesions demonstrate good demarcation with buckling of the subjacent cortex. Due to their slow-growing nature, there may be pressure erosion on the adjacent bone, in comparison to hyperostosis caused by meningiomas or bone destruction seen with metastatic disease.10 The T2- weighted images will show slightly higher signal intensity than typically seen with meningiomas, with patches of internal low signal. A “honeycomb” or “cord-like” appearance of enhancement is present, which is similar to the “rings and arcs” appearance seen on radiographs; meningiomas usually have a more homogeneous pattern of enhancement. The relative lack of surrounding edema distinguishes the lesion from metastatic disease.1,6,7 The absence of low signal on susceptibility or T2* images is not unusual, and thought to be related to well-differentiated cartilage with lack of gross calcification.1 Angiography can have a variable appearance, ranging from avascularity to intense hypervascularity that can be seen with an arteriovenous malformation or hemangiopericytoma.1,7
Due to the high risk of recurrence, aggressive local treatment is preferred with the goal of complete surgical resection. The use of adjuvant radiotherapy or chemotherapy is controversial, with some evidence that radiotherapy delays recurrence.6 Treatment with agents such as temozolomide and combination ifosfamide-doxorubicin has been reported in a few cases.11,12 Our patient was treated with complete resection, and no additional adjuvant therapy. Follow-up imaging has demonstrated no evidence of residual or recurrent tumor as of this report. The infrequent diagnosis of primary CNS chondrosarcoma makes it difficult to establish a standard protocol for treatment.
CONCLUSION
Primary intracranial extraskeletal chondrosarcoma, especially when dural based, is rare. Our case demonstrates that imaging findings can be confusing, and the diagnosis of a meningioma warrants consideration. However, key imaging features which may suggest chondrosarcoma are islands of low signal on T2 and a “honeycomb” or “cord-like” pattern of enhancement, both of which were present on this patient’s MRI exam. The correct diagnosis is important due to treatment/management implications. Once diagnosis is made, surveillance is important after initial treatment due to the high risk of recurrence, especially with the mesenchymal variant.
REFERENCES
- Kothari N, Law M, Cha S, Zagzag D. Conventional and perfusion MRI imaging of parafalcine chondrosarcoma. AJNR. 2003;24:245-248.
- Korten AG, Berg HJ, Spincemaille GH, van der Laan RT, Van de Wel AM. Intracranial chondrosarcoma: review of the literature and report of 15 cases. J NeurolNeurosurg Psychiatry. 1998;65:88-92.
- Oruckaptan HH, Berker M, Soylemezoglu F, Ozcan OE. Parafalcine chondrosarcoma: an unusual localization for a classical variant: case report and review of literature. Surg Neurol. 2001;55: 174-179.
- Vergeer RA, Vink R, Avenarius JK, Driesse MJ. A 71-year-old woman with an intracranial dural-based mesenchymal chondrosarcoma. Journal of Clinical Neuroscience. 2012;19:1170-1171.
- Hassounah M, Al Mefty O, Akhtar M, Jinkins JR, Fox JL. Primary cranial and intracranial chondrosarcoma: a survey. ActaNeurochir(Wien). 1985;78:123-132.
- Bosma JJD, Kirollos RW, Broome J, Eldridge PR. Primary intradural classic chondrosarcoma: Case report and literature review. Neurosurgery. 2001;48:420-423.
- Chandler JP, Yashar P, Laskin WB, Russell EJ. Intracranial chondrosarcoma: a case report and review of literature. Journal of Neuro-Oncology. 2004;68:33-39.
- Nagata S, Sawada K, Kitamura K. Chondrosarcoma arising from the falx cerebri. SurgNeruol. 1986;25:505-509.
- Scheithauer BW, Rubinstein LJ. Meningeal mesenchymal chondrosarcoma: report of 8 cases with review of the literature. Cancer. 1978;42:2744-2752.
- Lee YY, Van Tassel P, Raymond AK. Intracranial dural chondrosarcoma. AJNR. 1988;9:1189-1193.
- Aksoy S, Abali H, Kilickap S, Guler N. Successful treatment of a chemoresistant tumor with temozolomide in an adult patient: report of a recurrent intracranial mesenchymal chondrosarcoma. J Neurooncol. 2005;2:333-334.
- Sardi I, Massimino M, Genitori L, Buccoliero AM, Giangaspero F, Ferrari A. Intracranial mesenchymal chondrosarcoma: Report of two pediatric cases. Pediatr Blood Cancer. 2011;56:685-686.
Citation
AA B, N C, DF B. Primary intracranial extraskeletal chondrosarcoma. Appl Radiol. 2017;(2):32-34.
February 8, 2017