Primary Meningeal Rhabdomyosarcoma


Brought to you by Guerbet.
Case Summary
A 3-year-old previously healthy boy presented to the emergency room with a two-week history of worsening headaches and vomiting. The past medical history was non-contributory. Physical examination was unremarkable, with no focal neurological deficits. A noncontrast computed tomography (CT) scan of the brain was obtained as an initial study, followed by pre- and postcontrast magnetic resonance imaging (MRI) of the brain and spine for further evaluation.
Imaging Findings and Treatment
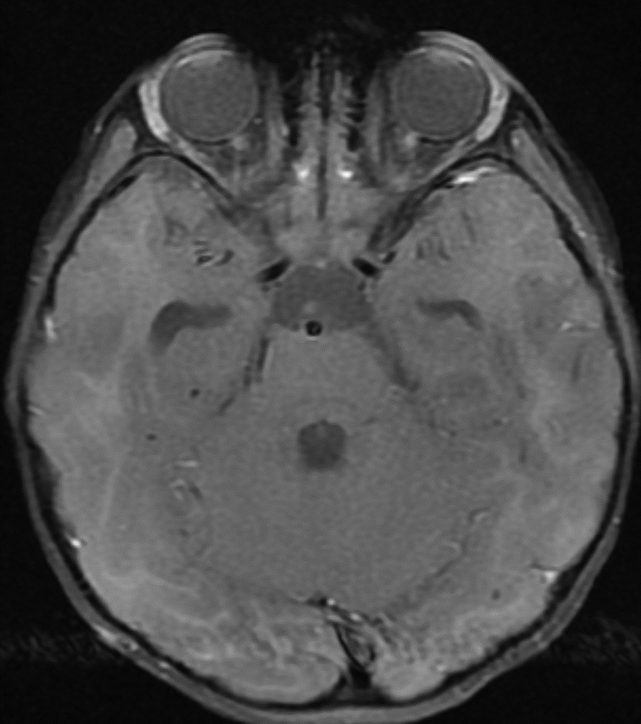
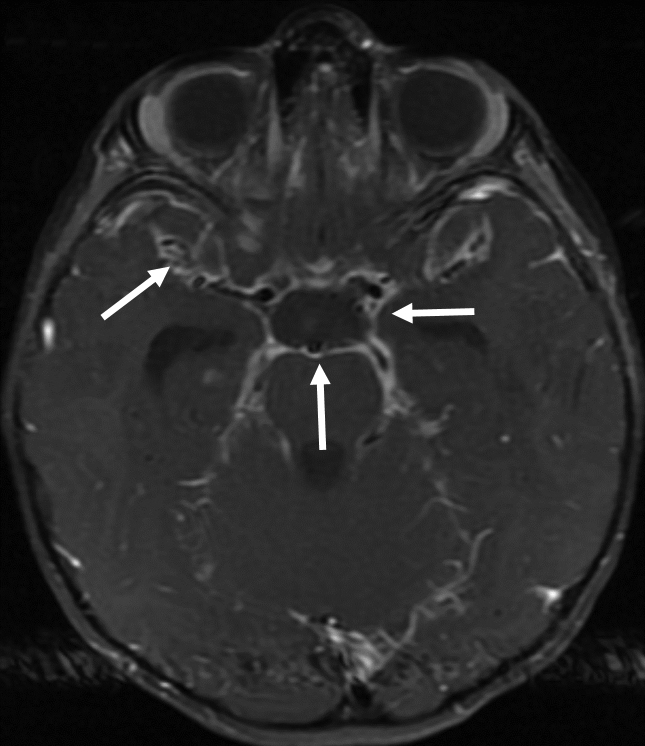
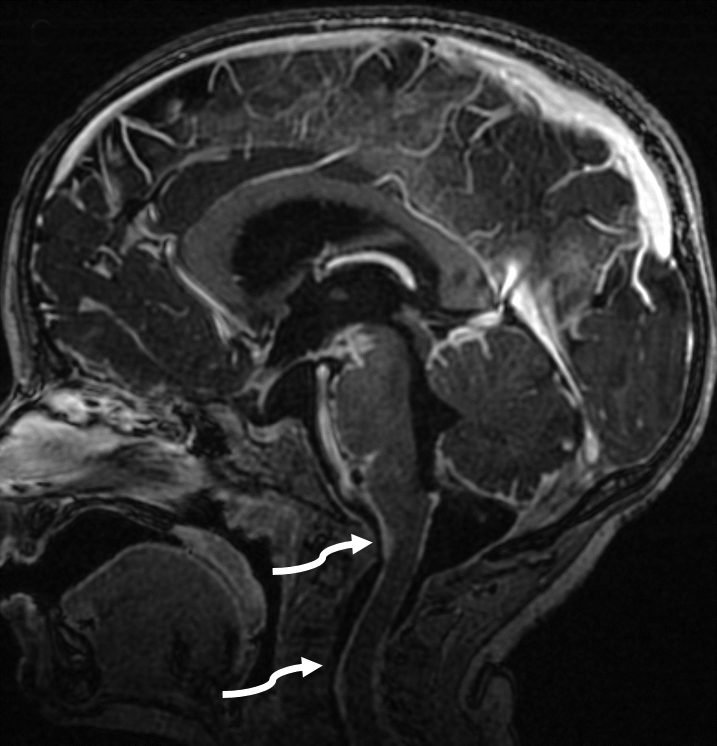
The initial noncontrast CT of the brain demonstrated mild enlargement of the ventricular system (not shown). Follow-up pre- and postcontrast MRI of the brain (Figure 1) demonstrated extensive, thick, and irregular leptomeningeal enhancement, most pronounced at the cranial base, basal cisterns, and Sylvian fissures. In addition, irregular leptomeningeal enhancement coated the brainstem and extended along the cervical spinal cord.
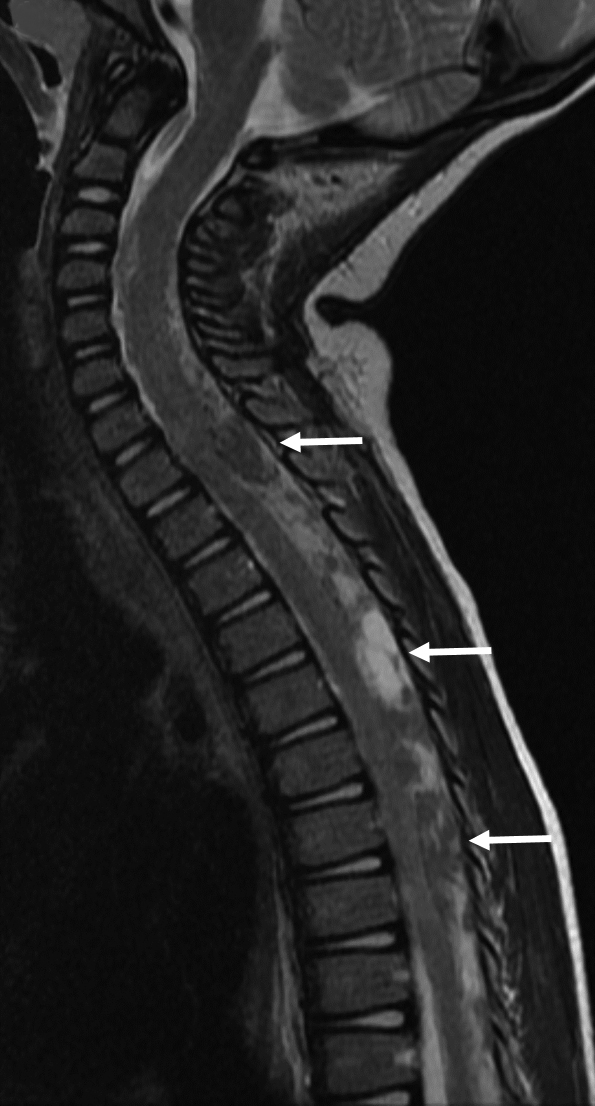
Concurrent MRI of the spine (Figure 2) demonstrated extensive, thick, heterogeneous, solid, and nodular enhancement within the thecal sac, causing mass effect with anterior displacement of the spinal cord. This thick nodular leptomeningeal enhancement encircled the cord and deformed its contour. There was also enhancement of the spinal nerve roots and the thickened cauda equina.
The imaging morphology suggested the possibility of neoplastic etiology, such as leptomeningeal metastasis over an infectious/inflammatory process such as tuberculosis and sarcoidosis. The patient underwent further work-up, including CT of the chest, abdomen, and pelvis, and a whole-body MRI study that did not demonstrate additional metastases or evidence of mass lesions.
The patient subsequently underwent endoscopic third ventriculostomy and external ventricular drain placement to relieve hydrocephalus, and biopsy of the arachnoid for histopathology. The biopsy sample consisted of rhabdomyoblasts ranging from spindled-strap to large eosinophilic cells and primitive ovoid cells in myxoid stroma. Immunohistochemistry revealed nuclear immunoreactivity for myogenin and myoD1, and cytoplasmic immunoreactivity for desmin. Findings were consistent with embryonal rhabdomyosarcoma.
Chemotherapy was initiated; however, the patient expired within a year of diagnosis from progressive disease in the brain and spinal cord.
Diagnosis
Primary meningeal rhabdomyosarcoma
Discussion
Rhabdomyosarcoma is the most common pediatric soft-tissue sarcoma, representing as much as 5% of all childhood malignancies, with a slight male preponderance and a mean age at diagnosis of 5-6 years.1,2 The most common sites of occurrence are the head and neck (orbits, non-parameningeal and parameningeal areas), genitourinary tract and extremities. Primary meningeal rhabdomyosarcoma is an extremely rare neoplasm with few cases reported in the literature.2-8
The major histological subtypes of rhabdomyosarcoma include the embryonal and alveolar, with the embryonal subtype accounting for approximately 70% of cases. Rare reported associations of rhabdomyosarcoma include neurofibromatosis type I, Li-Fraumeni syndrome, Gorlin basal cell nevus syndrome, and hypomelanosis of Ito.3
The histogenesis of intracranial sarcomas, notably the rhabdomyosarcomas, remains unclear. The pluripotent mesenchymal cells within the meninges are considered to be originator cells of various meningeal sarcomas.2,3However, interestingly, a primary meningeal rhabdomyosarcoma involving the meninges is more likely to originate from the brain parenchyma with meningeal extension than to be of de novo meningeal origin.3Distinguishing meningeal rhabdomyosarcoma from CNS tumors with rhabdomyoblastic differentiation such as teratomatous germ cell tumors and gliosarcoma is vital.2
As was the case with our patient, primary meningeal rhabdomyosarcoma most commonly presents with raised intracranial pressure resulting from hydrocephalus.3Diffuse involvement of the meninges, with thick, nodular, and irregular leptomeningeal involvement, termed as primary meningeal rhabdomyosarcomatosis, portends an extremely poor prognosis.3,9
The differential considerations on imaging for diffuse leptomeningeal thickening and enhancement include infections such as tuberculosis, and inflammatory pathologies such as sarcoidosis. However, profound thick and nodular enhancement with associated mass effect upon the spinal cord favors a neoplastic etiology.
Classifying these tumors as primary meningeal sarcomas is based primarily on radiologic and clinical findings, with a limited role for histopathology in differentiating primary from secondary neoplasms.3Based on lack of radiologic and clinical evidence of primary neoplasm outside the meninges, a primary meningeal rhabdomyosarcoma was considered in our case.
The prognosis of intracranial rhabdomyosarcoma remains dismal, with mean survival of 9.1 months.10The most common management approaches consist of chemotherapy, radiation and, when feasible, surgical resection.
Conclusion
Primary meningeal rhabdomyosarcoma is an extremely rare neoplasm with a dismal prognosis. Diffuse involvement of the meninges, with thick, nodular, and irregular leptomeningeal involvement, termed as primary meningeal rhabdomyosarcomatosis, portends an extremely poor prognosis.
References
- Jawad N, McHugh K. The clinical and radiologic features of paediatric rhabdomyosarcoma. Pediatr Radiol. 2019;49(11):1516-1523. doi: 10.1007/s00247-019-04386-5. Epub 2019 Oct 16. PMID: 31620851.
- Palta M, Riedel RF, Vredenburgh JJ, et al. Primary meningeal rhabdomyosarcoma. Sarcoma. 2011; 2011:312802. doi: 10.1155/2011/312802. Epub 2011 Jun 23. PMID: 21772793; PMCID: PMC3137955.
- Xu F, De Las Casas LE, Dobbs LJ Jr. Primary meningeal rhabdomyosarcoma in a child with hypomelanosis of Ito. Arch Pathol Lab Med. 2000;124(5):762-765. doi: 10.5858/2000-124-0762-PMRIAC. PMID: 10782165.
- Vuia O. Primary intracranial rhabdomyosarcoma producing proptosis. J Neurol Neurosurg Psychiatry. 1976;39(11):1143-1144. doi: 10.1136/jnnp.39.11.1143-a. PMID: 1011023; PMCID: PMC1083338.
- Kobayashi S, Hirakawa E, Sasaki M, Ishikawa M, Haba R. Meningeal rhabdomyosarcoma. Report of a case with cytologic, immunohistologic and ultrastructural studies. Acta Cytol. 1995;39(3):428-434. PMID: 7762328.
- Korinthenberg R, Edel G, Palm D, Müller KM, Brandt M, Müller RP. Primary rhabdomyosarcoma of the leptomeninx. Clinical, neuroradiological and pathological aspects. Clin Neurol Neurosurg. 1984;86(4):301-305. doi: 10.1016/0303-8467(84)90294-4. PMID: 6096065.
- Smith MT, Armbrustmacher VW, Violett TW. Diffuse meningeal rhabdomyosarcoma. Cancer. 1981;47(8):2081-2086. doi: 10.1002/1097-0142(19810415)47:8<2081::aid-cncr2820470829>3.0.co;2-1. PMID: 7194734.
- McCarville MB, Spunt SL, Pappo AS. Rhabdomyosarcoma in pediatric patients: the good, the bad, and the unusual. AJR Am J Roentgenol. 2001;176(6):1563-1569. doi: 10.2214/ajr.176.6.1761563. PMID: 11373233.
- Smith MT, Armbrustmacher VW, Violett TW. Diffuse meningeal rhabdomyosarcoma. Cancer. 1981;47(8):2081-2086. doi: 10.1002/1097-0142(19810415)47:8<2081::aid-cncr2820470829>3.0.co;2-1. PMID: 7194734.
- Celli P, Cervoni L, Maraglino C. Primary rhabdomyosarcoma of the brain: observations on a case with clinical and radiological evidence of cure. J Neurooncol. 1998;36(3):259-267. doi: 10.1023/a:1005884202389. PMID: 9524104.
