Radiological Case: Traumatic injury to the left internal mammary artery
Images


CASE SUMMARY
A 21-year-old, African-American male presented to the emergency department with a stab wound to the left chest. A 2-cm laceration with minimal oozing was noted on the anterior chest wall at the left lower-sternal border. On clinical assessment, the patient was hemodynamically stable and in no acute distress. A chest x-ray obtained at admission showed a normal cardiomediastinal silhouette with no lung or bone lesions. A computed tomography (CT) scan of the thorax with contrast demonstrated a large anterior mediastinal hematoma that was compressing the heart. Within the hematoma, a small region of arterial extravasation from injury to the left internal mammary artery (IMA) was identified. The patient underwent coil embolization of the left IMA to control the hemorrhage and thoracotomy for evacuation of the hematoma.
IMAGING FINDINGS
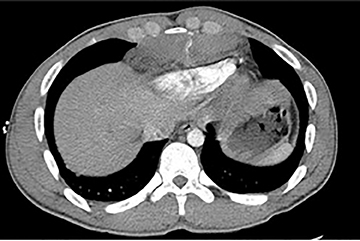
As a ligament injury was suspected to A CT scan of the thorax with contrast demonstrated a large anterior-mediastinal hematoma measuring 11 × 11 × 3.4-cm compressing the left ventricle. A small area of increased density within the hematoma suggested active extravasation of contrast material, indicating vascular injury (Figure 1). No hemothorax, pneumothorax, pleural or pericardial effusions were noted. Bony structures of the thorax were intact, with no evidence of acute fractures or dislocations. A small amount of air presentin the anterior and middle mediastinum was attributed to the stab wound.
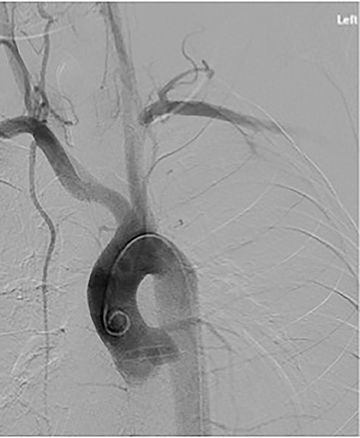
After accessing the right femoral artery with a micropuncture needle under ultrasound guidance, a thoracic aortogram was performed using a 5Fr pigtail catheter. Angiography of the aorta and its branches showed grossly normal vessels (Figure 2). A 5Fr Berenstein catheter was then used to perform a left subclavian arteriogram and an internal mammary artery catheter was used to perform a selective arteriogramo f the left IMA. Both studies demonstrated a focal area of extravasation in the distal left internal mammary artery corresponding to the area of enhancement identified on CT (Figure 3). A 3Fr microcatheter was used to place multiple 3-mm and 4-mm VortX Diamond coils (BostonScientific), both distal and proximal to the site of injury. A final arteriogram of the left IMA (Figure 4) showed successful resolution of the pseudoaneurysm with no residual flow. The following day, the hematoma was evacuated via thoracotomy to prevent infection. The patient tolerated the procedures well and there were no postoperative complications.
DIAGNOSIS
Traumatic injury to the left internal mammary artery (IMA)
DISCUSSION
Injury to the internal mammary artery is an uncommon cause of mediastinal hemorrhage after chest trauma and is often associated with other thoracic injuries. Prompt radiologic evaluation of the trauma followed by proper management can reduce mortality associated with the rare, but life-threatening complications of active IMA bleeding, such as hemorrhagic shock and cardiac tamponade1,2 Chest radiography,usually obtained for the initial evaluation of traumatic chest injury, may show a widened mediastinum, but the signs of hemorrhage may be nonspecific or obscured.3 CT with intravenous contrast is the more widely used imaging modality for accurately diagnosing thoracic trauma,especially vascular injuries and hemorrhage.2,3
CONCLUSION
Though surgical management is the standard treatment for IMA injuries, arterial embolization has been shown to provide a safe, less invasive alternative in select patients for achieving successful hemostasis, particularly in those who are not good candidates for surgery or have injuries that are not surgically accessible.2,4,5
REFERENCES
- Kwon OY, Chung SP, Yoo IS, et al. Delayed presentation of internal mammary artery rupture after blunt chest trauma: characteristic CT and plain x ray findings. Emergency Medicine Journal. 2005;22:664-665.
- Cagini L, Vanucci J, Scialpi M, Puma F. Diagnosis and endovascular treatment of an internal mammary artery injury. Journal of Emergency Medicine. 2013;44:117-119.
- Braatz T et al. CT diagnosis of internal mammary artery injury caused by blunt trauma. Clinical Radiology. 2001;56:120-123.
- Velmahos GC et al. Angiographic embolization for arrest of bleeding after penetrating trauma to the abdomen. American Journal of Surgery. 1999; 178: 367–373
- Kawamura S et al. Internal mammary artery injury after blunt chest trauma treated with transcatheter arterial embolization. The Journal of Trauma: Injury, Infection and Critical Care. 2006; 61:1536-1539.