Richter-type Spigelian hernia
Images



CASE SUMMARY
An 83-year-old woman presented to the emergency room with abdominal pain and vomiting. She had no previous history of abdominal surgery and no previous radiological images. Bowel sounds were increased. Blood tests showed increased inflammatory parameters (elevated acute phase reactants, leukocytosis and neutrophilia). The main clinical suspicion was acute diverticulitis.
IMAGING FINDINGS
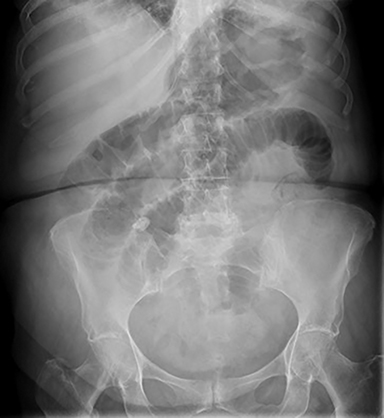
In abdominal radiography, distended small bowel loops were observed (several loops have a diameter greater than 3 cm). Distal aeration was present, existing air bubbles in the rectum. Given these findings, a diagnosis of sub-occlusive ileus or progressive occlusive ileus was established (Figure 1).
Despite the use of gastric tube and analgesia, abdominal pain continued. An abdominal CT scan with intravenous contrast was performed.
Computerized tomography showed dilated small bowel loops without affecting the colon. There was a transition point in the ileum. There, the antimesenteric side of the ileum was herniated (Richter’s hernia) through a defect in the abdominal wall located in the inferior third of the left semilunar line (Spigelian hernia).
Herniated ileum showed wall edema and surrounding free fluid (Figure 2). Contrast enhancement was preserved or even increased, indicating that there was no arterial compromise, but only venous compromise. As an incidental finding a liquid collection in left inguinal region was identified. It measured about 5 cm and is related to a previous left inguinal hernia repair.
Taking into account these findings, the surgery department performed laparoscopic ventral hernia repair. The patient progressed appropriately.
DIAGNOSIS
Antimesenteric hernia portion of the small intestine (Richter’s hernia) through the left semilunar line of the abdomen (Spigelian hernia).
DISCUSSION
Although they are two relatively common entities, the fact that both phenomena can occur simultaneously (Richter’s herniation through Spigelian line) is very unusual. A literature review conducted in 2014 found only six cases since 1978.1
Spigelian hernias occur through a defect in the linea semilunaris, a fibrous union of the rectus sheath with the aponeuroses of the transverse abdominal and abdominal internal oblique muscles that extends from the level of the ninth rib cartilage to the pubic symphysis. Usually wall defects are secondary to acquired weakness of the abdominal wall, often related to surgical incisions.2
This is a rare type of abdominal wall hernia. A literature review found just 479 cases reported between 1970 and 2000.3
Diagnosing Spigelian hernia clinically is difficult because it produces nonspecific symptoms.4 The most common is pain in the location of the hernia. Herniation may be apparent on clinical exam or ultrasound in some patients. Nevertheless, abdominal CT with intravenous contrast is the imaging test of choice because it reveals vascular compromise or other underlying pathology.
Immediate treatment is recommended because of the high risk of incarceration, in approximately 24% of cases, and the low risk of recurrence if the procedure is properly done.5
On the other hand, Richter’s hernia results in strangulation of only a part of the bowel wall circumference in a hernia sac. It occurs more commonly in the femoral region, it is more frequent in women and it usually involves a segment of distal ileum.6
Since only one side of the intestine is affected, the obstruction is rare. This type of hernia is usually found incidentally, but intestinal necrosis and perforation can occur.
The treatment of choice for Spigelian and Richter’s hernias is laparoscopic mesh repair of the abdominal wall defect.7 If intestinal necrosis is established, the affected segment must be resected.
CONCLUSION
Spigelian hernia is a rare type of abdominal wall hernia that is difficult to diagnose clinically. On the other hand, it is even more uncommon to find a hernia that only affects the antimesenteric side of the bowel in that location.
Computed tomography with intravenous contrast is the imaging technique of choice for the diagnosis of this entity to determine the extension and severity of bowel impact. The findings in this imaging test determine the treatment and prognosis.
REFERENCES
- Foster D, Nagarajan S, Panait L. Richter-type Spigelian hernia: A case report and review of the literature. Int J Surg Case Rep. 2014 Dec 11;6:160–162.
- Larson D.W. and Farley D.R. Spigelian hernias: repair and outcome for 81 patients. World J Surg. 2002;26:1277–1281.
- Fisichella PM, Harwell J, Brosnan J, Abcarian H. Richter’s hernia through a Spigelian defect of the abdominal wall. The American Journal of Surgery. 2007 Jan 1;193(1):69–70.
- Moreno-Egea A, Flores B, Girela E, Martín J, Aguayo J, Canteras M. Spigelian hernia: bibliographical study and presentation of a series of 28 patients. Hernia. 2002 Dec 1;6(4):167–170.
- Baucom C, Nguyen QD, Hidalgo M, Slakey D. Minimally invasive spigelian hernia repair. JSLS. 2009;13(2):263–268.
- Parambath AN, Hajaji K, Hilil SAA. Spigelian hernia with Richter-type herniation of the ileum: A rare cause of right iliac fossa pain mimicking acute appendicitis. ResearchGate. 2012 Dec 1;2012(2012):7.
- Moreno-Egea A, Carrasco L, Girela E, Martín J-G, Aguayo JL, Canteras M. Open vs laparoscopic repair of spigelian hernia: a prospective randomized trial. Arch Surg. 2002;137:1266–1268.
Citation
J D, S A, C B, N N, J S, J P. Richter-type Spigelian hernia. Appl Radiol. 2018;(5):42-43.
May 8, 2018