Septic Arthritis with Osteomyelitis
Images

Case Summary
A child with a history of global developmental delay, infantile spasms, and seizures presented from an orthopedic clinic with a one-week history of progressively worsening left-sided limp and non-weight bearing. Acetaminophen and ibuprofen did not improve the symptoms.
On physical exam, the patient’s left hip joint was tender to palpation with limited range of motion in all planes. Laboratory studies showed elevated C-reactive protein (CRP; 0.80 mg/dL), elevated erythrocyte sedimentation rate (ESR; 28 mm/hr), normal white blood cell count (WBC; 7,500 µL), and left shift with elevated immature granulocytes (0.4%).
Imaging Findings
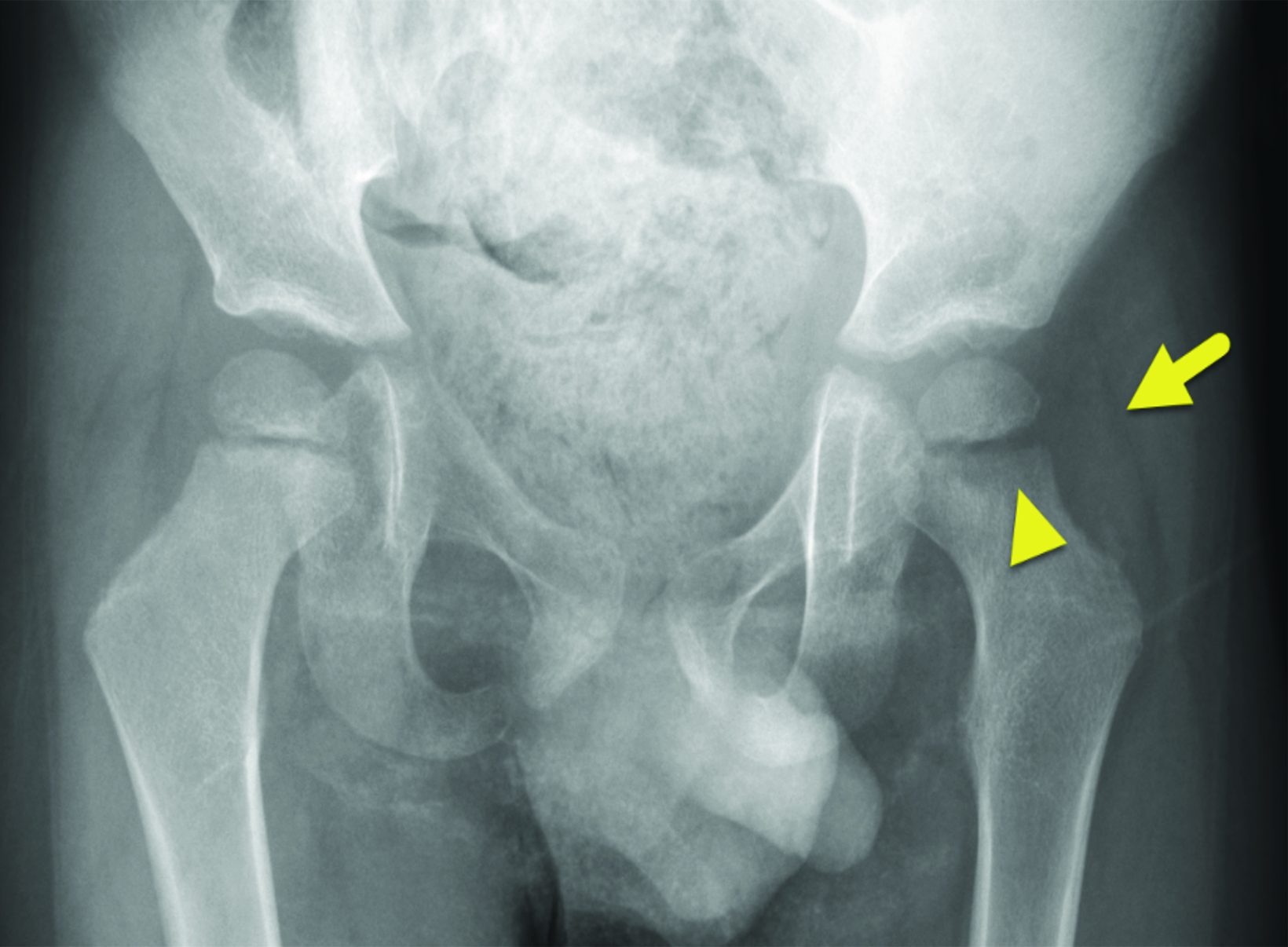
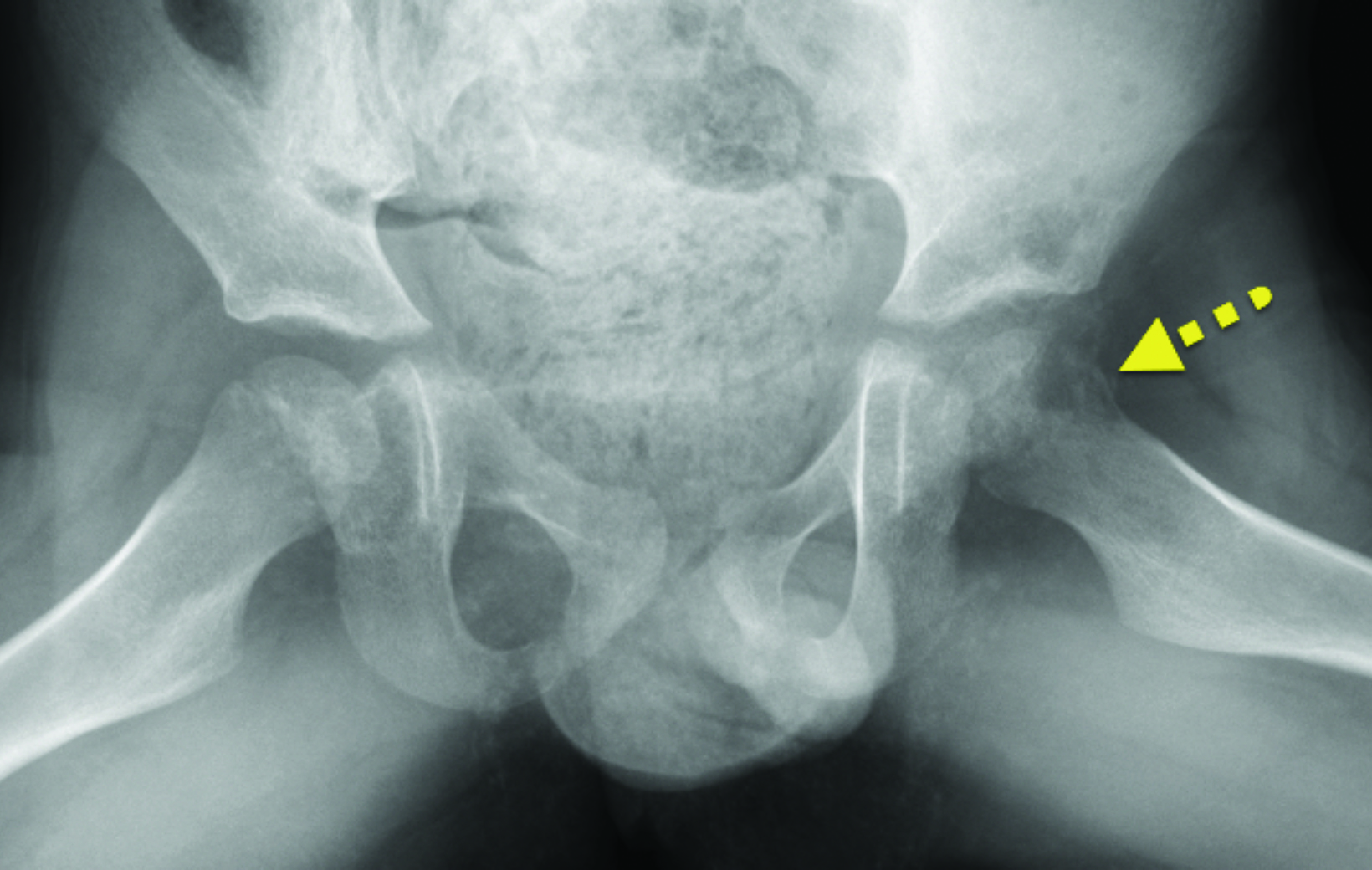
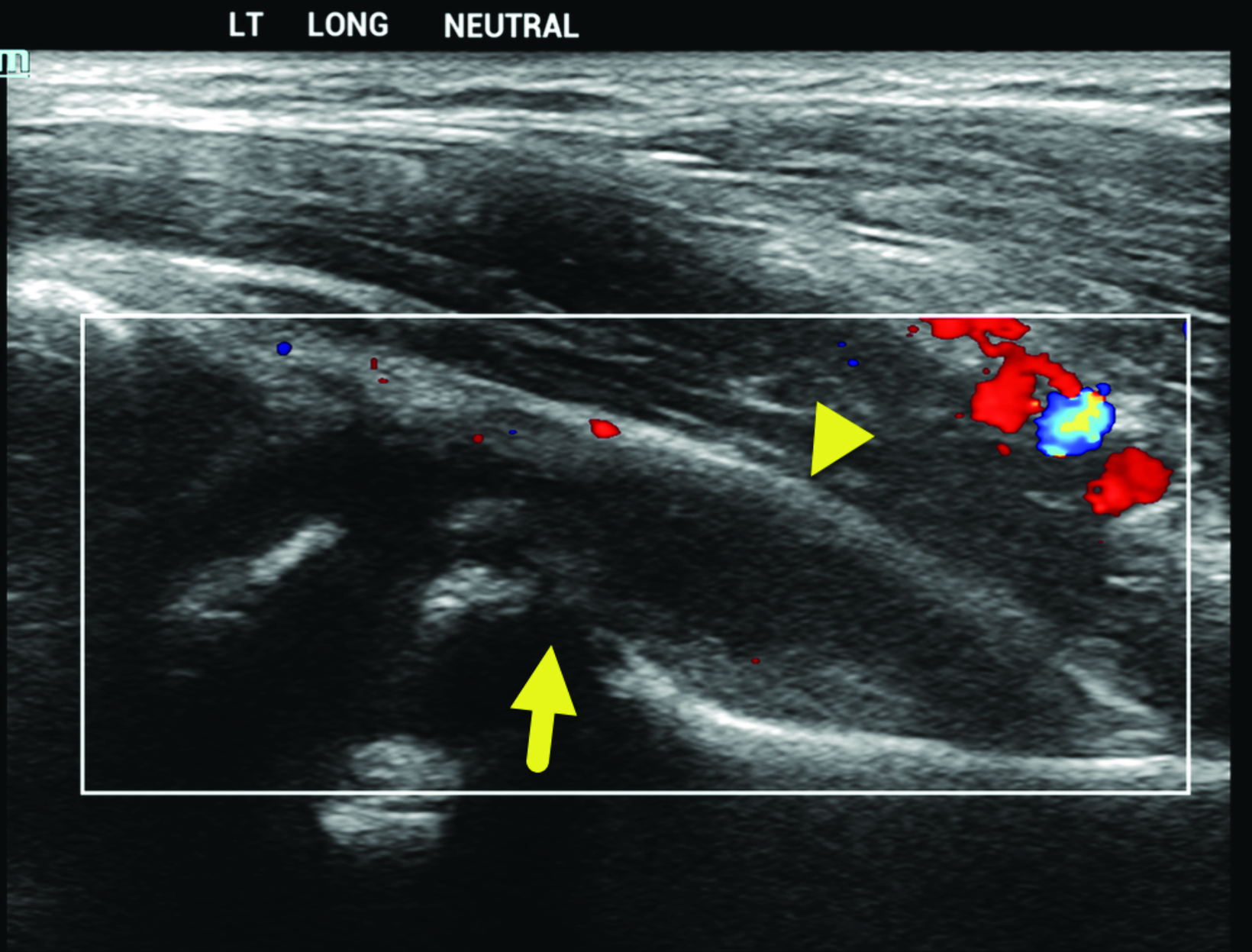
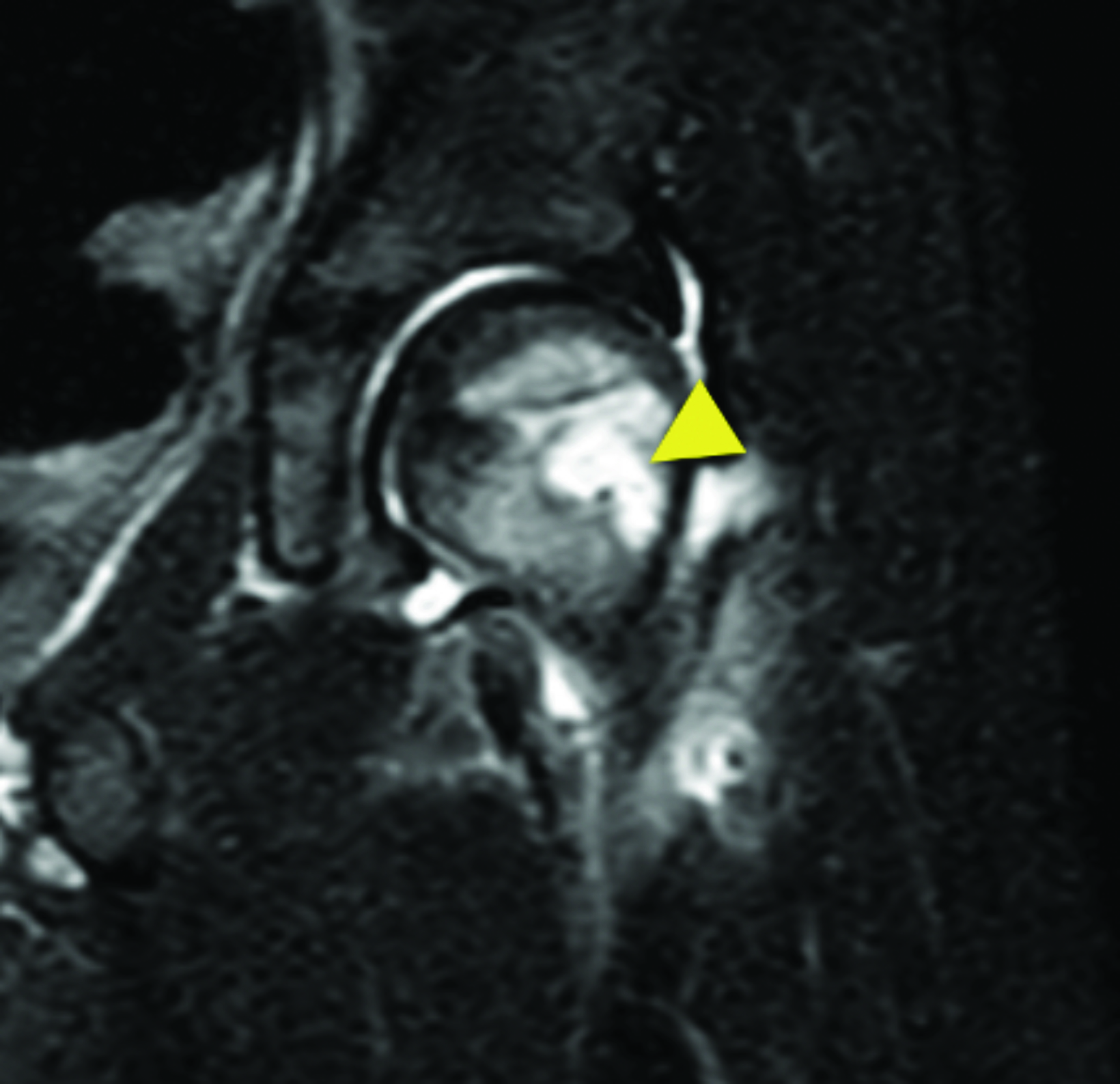
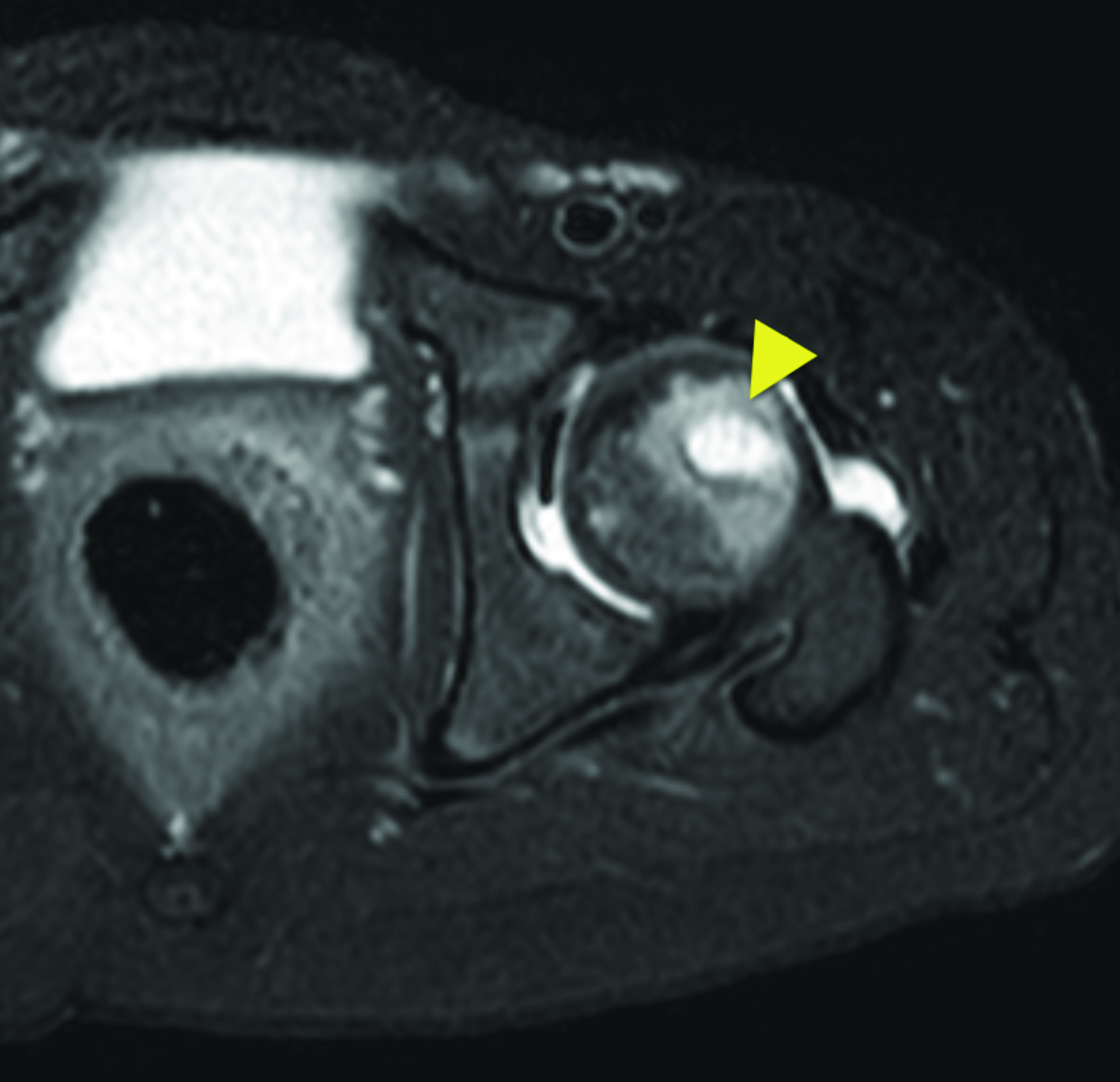
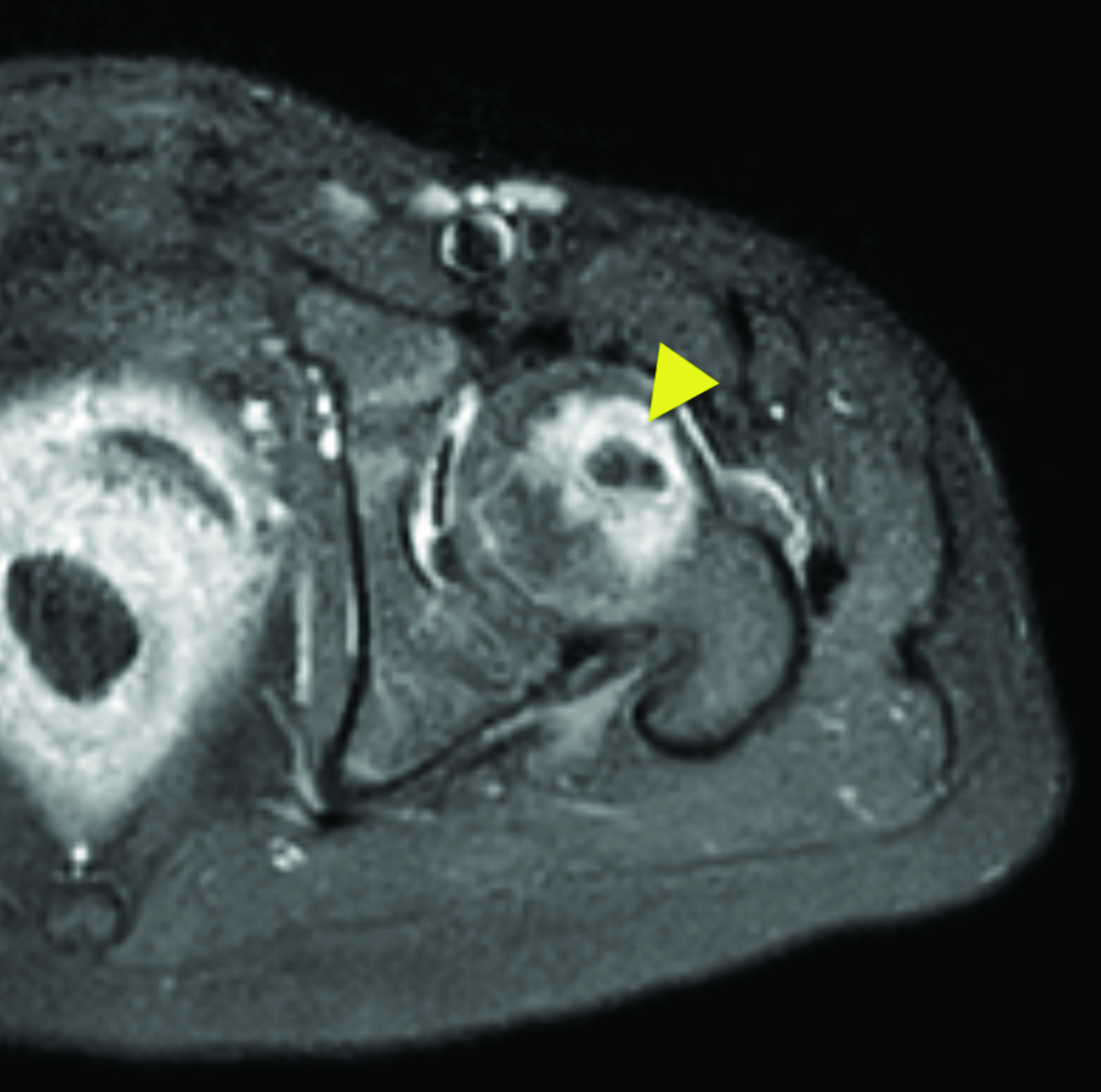
Initial radiograph of the hips (Figure 1) showed a left-hip effusion, widening of the proximal femoral physis, and lucency in the lateral aspect of the femoral metaphysis. An ultrasound confirmed the left-hip effusion and showed regions of cortical destruction (Figure 2). Subsequent magnetic resonance imaging (MRI) of the left hip showed edema within the proximal left femur, an intramedullary abscess, and a small hip effusion (Figure 3).
Diagnosis
Septic arthritis with osteomyelitis.
Differential diagnoses for children with a limp include transient synovitis (also known as toxic synovitis), fracture, Legg-Calve-Perthes disease, and malignancy.
Discussion
Septic arthritis results from an infection of the synovial fluid within the joint space1. In children, it most commonly occurs secondary to hematogenous spread of infection. However, the joint can also become directly infected from adjacent osteomyelitis or a puncture wound.2,3
The overall incidence of acute septic arthritis in the US is 4-10 per 100,000 children,4 with boys affected twice as often as girls. Most cases are monoarticular, with 80% arising in the large joints of the lower extremity.5 Signs and symptoms include joint pain and tenderness, redness, swelling, warmth, and restricted movement. Risk factors include history of bacteremia, pre-existing joint disease, and immunosuppression.
Septic arthritis in children under 2 months of age is often caused by Staphylococcus aureus, Escherichia coli, group B streptococci, and other gram-negative bacilli. Neonates are relatively immune incompetent, may not localize infection well, and may develop multifocal infection. In children 2 months to 5 years, the most common etiologies are Haemophilus influenzae type B, Staphylococcus aureus, Group A streptococci, and Streptococcus pneumoniae. In adolescents, typical organisms include Neisseria gonorrhoeae and Group A streptococcus. Less common pathogens include Mycobacterium tuberculosis, Kingella kingae, Borrelia burgdorferi, fungi such as Coccidioides immitis or Histoplasmosis capsulatum, and viruses such as rubella, parvovirus B19, and varicella zoster virus.6
Diagnosing septic arthritis begins with a thorough history and physical examination to identify joint and/or bony pathology. In children with refusal to bear weight, the differential diagnosis typically includes septic arthritis and transient synovitis. Both conditions lead to synovial inflammation and joint effusion formation. However, septic arthritis can result in joint destruction and requires urgent hip joint decompression and intravenous antibiotics, whereas transient synovitis is benign and self-limiting without long-term sequalae.
The Kocher criteria use clinical and laboratory data to differentiate septic arthritis from transient synovitis. Septic arthritis is suspected if a patient has a fever > 38.5°C, is non-weight bearing, has an ESR >40 mm/hr; WBC >12,000 cells/µL, or CRP > 20mg/L.1 The more of these criteria that are positive, the higher the diagnostic specificity.
Imaging begins with radiographs. Radiography helps to identify potential causes of pain, including osteomyelitis, fracture, or neoplasm. Specific findings of septic arthritis on radiography may include joint destruction or irregularities, subluxation, and dislocation. In cases with
joint effusion, increased joint space diameter may also be appreciated. Radiographs are most useful for detecting processes after 7-10 days, as acute findings may be absent earlier in the disease.6 Because radiographs may be normal early in the course of infection, other imaging modalities should be added if infection remains in the differential diagnosis.
Ultrasound is sensitive for joint effusions and can be used to guide joint aspiration. When performing ultrasound, it is important to understand that absence of an effusion does not exclude septic arthritis, and that ultrasound cannot reliably distinguish a septic effusion from a noninfected effusion. Occasionally, however, features such as a cortical destruction are present and allow for a confident diagnosis of septic arthritis related to osteomyelitis.
Magnetic resonance imaging is sensitive for infection within the bone and soft tissue.7 Typically, infection appears as low-signal intensity on T1 images and high signal on T2 images. Enhancement characteristics can be variable. Differences in the enhancement pattern may be related to factors such as the pathogen or the presence of abscess. While MRI cannot distinguish whether a joint effusion is infected, features that favor septic arthritis include the presence of bone marrow or soft tissue edema and decreased enhancement of the epiphysis of the affected bone.
Suspected septic arthritis should be treated emergently, as cartilage and bone destruction can occur within days. Initial blood studies and cultures should be obtained and diagnosis confirmed by a joint aspiration. Joint fluid, if present, should be collected and sent for cultures and laboratory analysis with microscopic examination for white cells, gram stain, and culture for organisms. All joint fluid should be aspirated to reduce the joint pressure and number of organisms.
Treatment includes joint aspiration via needle, arthroscopy, or open arthrotomy. Empiric antimicrobial therapy should be started to cover most pathogens. Once susceptibility data becomes available a more specific antibiotic therapy should be initiated.8 A 6-week clinical and radiological follow-up examination is recommended to evaluate for residual infection and potential complications.
Conclusion
Septic arthritis is a medical emergency. While imaging can play a role in its diagnosis, clinical and laboratory criteria are often used to guide management and imaging decisions. Joint aspiration is required for diagnosis and targeted antibiotic therapy.
References
- Wall C, Donnan L. Septic arthritis in children. Aust Fam Physician. 2015;44(4): 213-215.
- Mader JT, Shirtliff M, Calhoun JH. The host and the skeletal infection: Classification and pathogenesis of acute bacterial bone and joint sepsis. Baillieres Best Pract Res Clin Rheumatol. 1999;13(1):1-20. doi: S1521-6942(99)90003-7 [pii].
- Xu C, Peng H, Li R, et al. Risk factors and clinical characteristics of deep knee infection in patients with intra-articular injections: A matched retrospective cohort analysis. Semin Arthritis Rheum. 2018;47(6):911-916. doi: S0049-0172(17)30508-5 [pii].
- Arnold JC, Bradley JS. Osteoarticular infections in children. Infect Dis Clin North Am. 2015;29(3):557-574. doi: S0891-5520(15)00061-6 [pii].
- Baitch A. 15 recent observations of acute suppurative arthritis*. Clinical Orthopaedics and Related Research®. 1962;22. https://journals.lww.com/clinorthop/Full- text/1962/00220/15_Recent_Observations_of_Acute_Suppurative.15.aspx.
- Montgomery NI, Epps HR. Pediatric septic arthritis. Orthop Clin North Am. 2017;48(2):209-216. doi: S0030-5898(16)30164-X [pii].
- Agarwal A, Aggarwal AN. Bone and joint infections in children: Septic arthritis. Indian J Pediatr. 2016;83(8):825-833. doi: 10.1007/s12098-015-1816-1.
- Sharff KA, Richards EP, Townes JM. Clinical management of septic arthritis. Curr Rheumatol Rep. 2013;15(6):332-4. doi:10.1007/s11926-013-0332-4.
References
Citation
JK T, RB T, CM S, Y L, AJ T. Septic Arthritis with Osteomyelitis. Appl Radiol. 2022;(3):56A-56C.
April 26, 2022