Spontaneous aorta-left renal vein and #64257;stula



Prepared by Deborah J. Conway, MD and Michael P. Carter, MD from the Department of Radiology,Memorial Health University Medical Center, Savannah, GA. Dr. Conway is now a Pediatric RadiologyFellow at Children's Hospital, Seattle, WA.
CASE SUMMARY
A 73-year-old white male whocomplained of abdominal pain underwent a contrast-enhanced computed tomography (CT) examination of the abdomen (Figure 1). Thisstudy revealed an infrarenal abdominal aortic aneurysm measuring 8 cm in greatest anteroposterior diameter. Contrastopacification of both kidneys was shown on this CT.
Five days later, the patient developed anelevated serum creatinine level as well as high-output congestive failure. Another CT of the abdomen was performed (Figure 2) thatdemonstrated opacification of the aorta, inferior vena cava (IVC), and left renal vein to the same degree with intravenouscontrast with near absent perfusion of the left kidney.
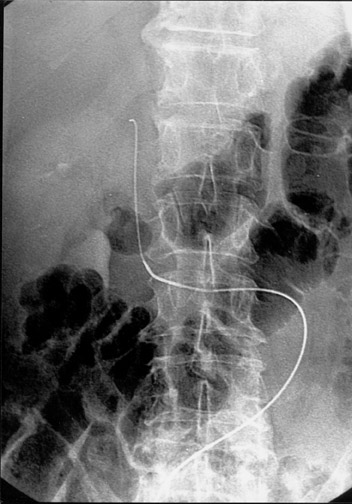
The patient underwent aortography. A floppyJ-wire was inserted through the aortic aneurysm into the left renal vein and subsequently into the IVC (Figure 3). Followingcontrast administration, there was rapid visualization of the left renal vein as well as the IVC (Figure 4).
DIAGNOSIS
Spontaneous aorta-left renal veinfistula
IMAGING FINDINGS
An abdominal CT obtainedupon the patient's initial presentation to an outside facility shows a fusiform abdominal aortic aneurysm with focal contourdeformity posteriorly, anterior to a retroaortic left renal vein (Figure 1). There is contrast opacification of the aorta,left renal vein, and IVC to the same degree; both kidneys are perfused. A second abdominal CT obtained 5 days following the initialpresentation again reveals focal contour abnormality of the posterior abdominal aortic aneurysm directly anterior to the left renalvein with enhancement of the aorta, IVC, and left renal vein to the same degree; however, the left kidney is now minimally perfused(Figure 2). An abdominal aortogram obtained upon presen-tation to our facility demonstrates passage of a wire into the rightfemoral artery, through the fistula, into the left renal vein and, finally, into the IVC (Figure 3). Contrast injectedinto the upper abdominal aorta is immediately seen within the aorta, left renal vein, and IVC simultaneously, showing thefistula between the aorta and left renal vein (Figure 4).
DISCUSSION
Many complications of abdominalaortic aneurysm have been described, the most common being rupture. A less commonly described complication is the development of afistula from the enlarged aorta to other nearby structures. A number of cases of aorta-caval fistulas have beendescribed in medical literature. Iliac vein and enteric fistulas have also been described. Other vascular communications arefar less common. This case demonstrates the spontaneous development of a fistula between an abdominal aortic aneurysm and aretroaortic left renal vein. An English literature search revealed only 20 reported cases 1-19 of spontaneous aorta-left renal vein fistula; however, none of these reports indicated the evolution ofsuch a fistula with radiographic imaging. Almost all of these patients had a retroaortic left renal vein. 1
Prior reports have described a clinical syndrome of abdominal pain,pulsatile abdominal mass, elevated serum creatinine, hematuria, and nonperfusion of the left kidney on imaging studies. 2 Often, as serum creatinine rises due to nonperfusion of the left kidney, treatment is delayed asa primary renal problem is suspected. 3 Also, physicians are reluctant to perform a CT ofthe abdomen with contrast due to poor renal function, again delaying the diagnosis.
Sultan et al 20 describe an attempt at endovascular repair with a stent graft that, although it was unsuccessfulin that particular case, suggests a minimally invasive approach might be used in the future.
CONCLUSION
Although an aorta-left renal veinfistula is a rare entity, this diagnosis must be suspected in a patient with abdominal aortic aneurysm, hematuria, andworsening renal function. Also, endovascular repair should be considered, especially in patients with a high surgical risk.
