Urachal adenocarcinoma
Images
CASE SUMMARY
A 49-year-old male presented to his primary care physician with painless, gross hematuria. Initial evaluation included physical examination, urinalysis, urine cytology and a CT urogram followed by a urologic consultation. Physical examination identified no specific abnormality, including no palpable masses or umbilical discharge. Aside from confirming the hematuria was non-contributory, urine cytology demonstrated the presence of atypical cells, raising concern for malignancy and prompting imaging evaluation. CT urogram demonstrated a midline bladder dome mass with perivesical extension. This was followed by transurethral resection of bladder tumor (TURBT) and ultimately a partial cystectomy.
IMAGING FINDINGS
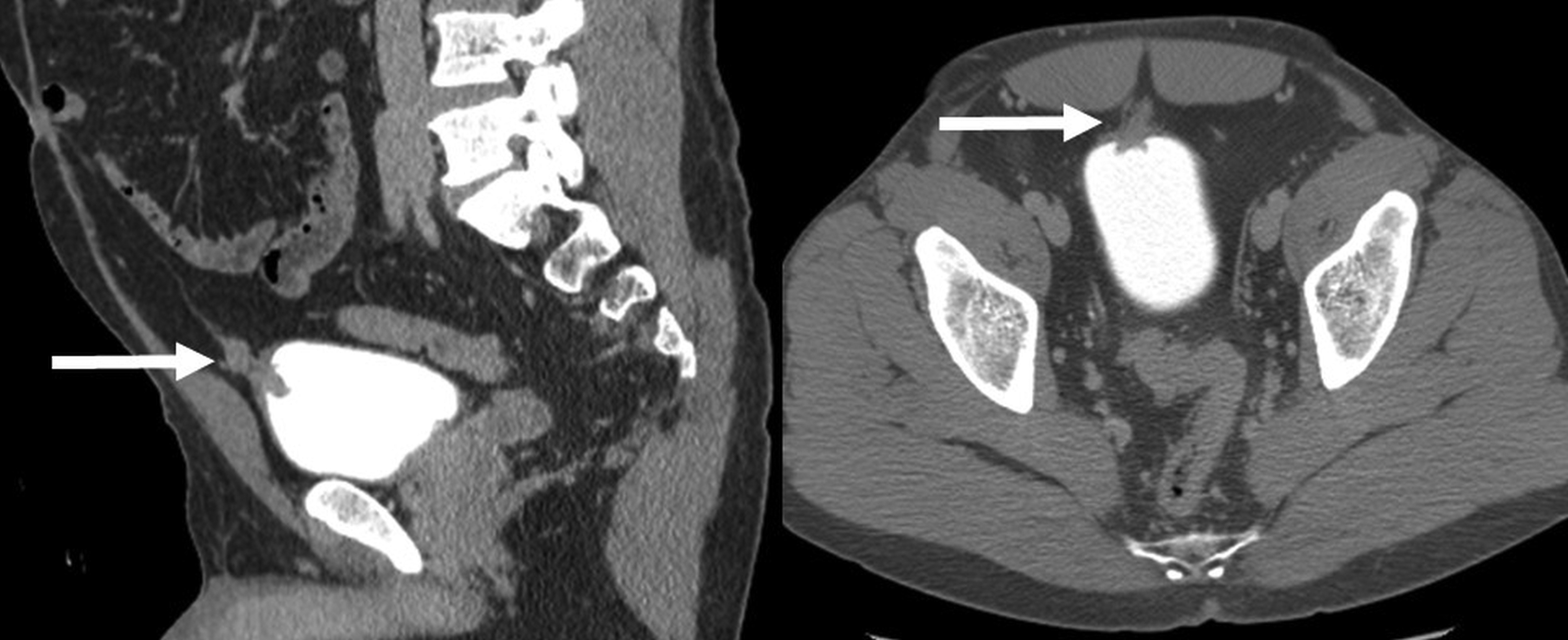
CT urogram demonstrated a midline bladder dome mass with perivesical extension (Figure 1). No calcification was identified within the mass. No synchronous lesions were seen elsewhere in the bladder or collecting systems. No adenopathy was present.
DIAGNOSIS
Urachal adenocarcinoma. Differential diagnosis includes urothelial carcinoma.
DISCUSSION
The urachus, or median umbilical ligament, is a derivative of the embryological cloaca and allantois. It initially forms as a tubular structure but involutes before birth and remains as a fibrous band that connects the apex of the bladder dome to the umbilicus.1 Malignant urachal neoplasms can arise from an urachal remnant but are rare and represent less than 1% of all bladder cancers,1 yet 34% of all bladder adenocarcinomas are urachal in origin. The urachus is lined by transitional epithelium, yet urachal carcinoma manifests as adenocarcinoma in 90% of cases.1 Adenocarcinoma of the bladder is also associated with bladder exstrophy.
Urachal tumors are most commonly found in patients aged 40-70 years, and two-thirds of these cases occur in men.1 The prognosis is related to the stage and degree of differentiation; however, due to their extraperitoneal location, they may be clinically silent and manifest only when invasion or metastatic disease occurs.1 In these cases, prognosis is generally poor, with a 5-year survival rate of 6.5 -15%.1
The most common clinical symptoms described with urachal adenocarcinomas include hematuria, dysuria, urinary frequency, urinary urgency, and pain. The only curative treatment is surgical excision, which may provide long-term survival if the tumor is detected early.
The portion of the urachus adjacent to the dome of the bladder is the most common location for urachal carcinomas to arise and represents 90% of cases. The tumor can extend superiorly toward the umbilicus, and inferiorly through the bladder wall. Less frequently, carcinoma can occur in the middle of the urachus or closer to the umbilical end.1
CT imaging may demonstrate solid, cystic, or mixed features of the tumor. Mucin production is common and can be identified as low-attenuation components on CT (60% of cases) or as increased echogenicity on ultrasound.1 As with other adenocarcinomas of the abdomen, calcifications are often present in urachal adenocarcinomas and are identified in 50-70% of cases. They can be punctate, stippled, curvilinear and peripheral, or psammmomatous on CT.1 The finding of calcifications in a midline supravesical mass is considered nearly pathognomonic for urachal adenocarcinoma.1
MRI may demonstrate high signal intensity on T2-weighted images due either to mucin content or to necrosis.2 Solid components of the tumor may be isointense with soft tissue on T1-weighted images, and enhance with gadolinium administration.
Urachal carcinoma is difficult to distinguish from the uncommon primary bladder adenocarcinoma on histological analysis alone. On CT, however, the bulk of a urachal tumor is usually found to have a larger extravesicular component and tends to grow toward the umbilicus in the perivesical space.1,3 In primary bladder adenocarcinoma, a larger intravesicular component without perivesical extension is much more typically seen.
Urachal adenocarcinoma can be difficult to distinguish radiologically from an infected urachal cyst, as both may appear as mixed cystic/solid masses in the pathway of the urachal remnant. Urachal cysts are generally asymptomatic congenital anomalies of the urachus, but they can become infected or give rise to malignancy and lead to their detection. A location near the bladder dome favors a urachal cancer. It may be important to include an urachal cyst in the differential diagnosis when considering urachal adenocarcinoma given an appropriate clinical picture.
CONCLUSION
Urachal origin adenocarcinoma is a rare neoplasm but has a near pathognomonic appearance that allows the radiologist to confidently suggest the diagnosis prospectively. A soft-tissue mass arising in the midline near the bladder dome is highly suggestive of a urachal adenocarcinoma. The presence of calcifications is the lesion is an additional finding that will strengthen the confidence of diagnosis. Prospectively identifying this diagnosis allows the urologist to guide therapy to partial or complete cystectomy, as these lesions are not successfully treated with TURBT, which is more commonly utilized in conventional urothelial cancer.
REFERENCES
- Yu, JS, et al. Urachal remnant diseases: spectrum of CT and US findings. Radiographics. 2001; 21(2): 451-461.
- Parada Villavicencio, C, et al. Imaging of the urachus: anomalies, complications, and mimics. Radiographics. 2016; 36(7): 2049-2063.
- Thali-Schwab CM, Woodward PJ, and Wagner BJ. Computed tomographic appearance of urachal adenocarcinomas: review of 25 cases. Euro Radiol. 2005; 15(1): 79-84.
Citation
V V, DT M.Urachal adenocarcinoma. Appl Radiol. 2019; (5):44-45.
September 25, 2019