Autoimmune Hepatitis
By Saeed O, Towbin RB, Towbin AJ



CASE SUMMARY
An 11-year old being treated with bupropion for major depressive disorder and other psychiatric illnesses presented after routine laboratory monitoring identified persistently elevated liver enzymes, hyperbilirubinemia, hyperammonemia, thrombocytopenia, hypoalbuminemia, and an abnormal International Normalized Ratio (INR).
IMAGING FINDINGS
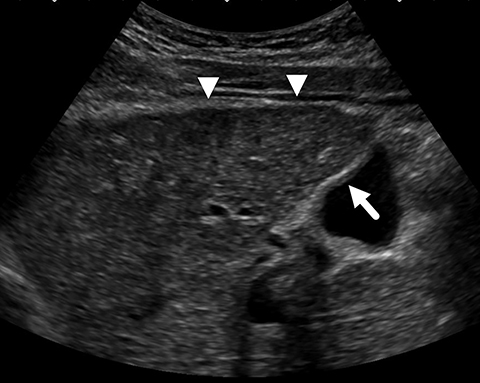
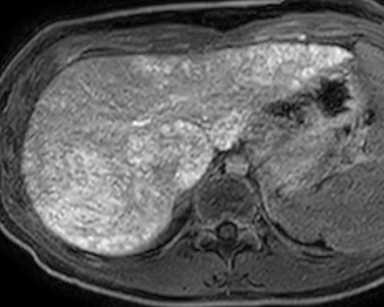
An initial ultrasound scan revealed a diffusely coarsened and heterogenous echotexture throughout the liver with a nodular contour but no discrete mass (Figure 1). In addition to the abnormal hepatic parenchyma, there was mild gallbladder wall thickening with sludge in the lumen, splenomegaly, and prominent porta hepatis lymph nodes.
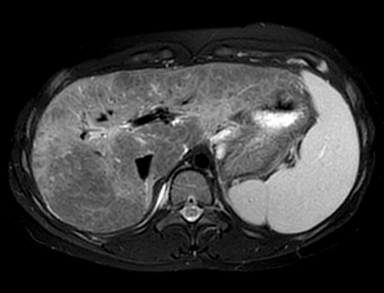
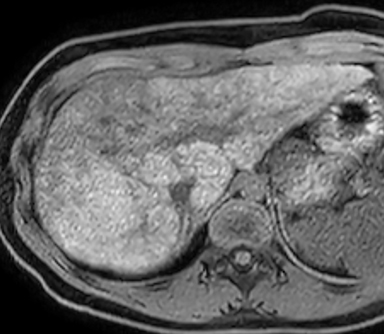
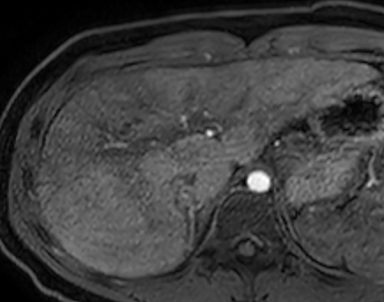
Magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatography (MRCP) of the abdomen performed before and after administration of gadoxetate disodium (Eovist/Primavist; Bayer, Leverkusen, Germany) showed the liver to have a lobulated contour with several discrete nodules and diffuse abnormal reticular increased T2/decreased T1 signal typical of hepatic fibrosis (Figure 2). Postcontrast images showed no worrisome nodules during the hepatic arterial and portal venous phase of imaging.
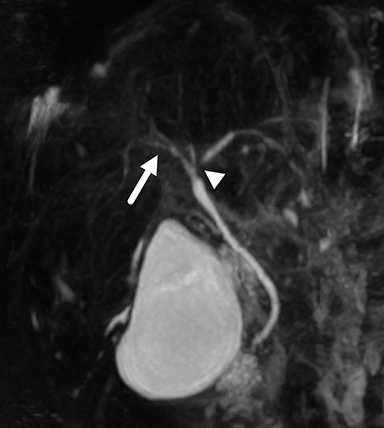
The liver, however, appeared markedly abnormal on the hepatobiliary phase of imaging with diffuse reticular areas that did not retain contrast. MR elastography demonstrated a mean stiffness of 7.26 kPa (normal <2.71 kPa). MRCP showed irregularity in the central intrahepatic bile ducts. The common bile duct had a normal, smooth appearance. Notably, hepatic fat content and iron content were both normal at 3% (normal being < 5%) and 1073 mcg/g dry weight (normal being 400-1600 mcg/g dry weight) respectively. An ultrasound-guided percutaneous liver biopsy was performed.
DIAGNOSIS
Autoimmune hepatitis (AIH). The differential diagnosis for cryptogenic cirrhosis in a child includes nonalcoholic steatohepatitis, autoimmune hepatitis, sclerosing cholangitis, drug-induced hepatitis, and Wilson disease.
DISCUSSION
Autoimmune hepatitis is an immune-related chronic liver disorder of unknown etiology characterized by hepatocellular inflammation with progression to cirrhosis. The disorder was first termed “chronic hepatitis” by Waldenstrom in 1950 as he appropriately disassociated it from infectious hepatitis.1 The prevailing thought at the time was that chronic hepatitis was a sequela of acute infectious hepatitis. While this hypothesis has since been disproven, Waldenstrom correctly noted the chronic inflammatory cell infiltration and hypergammaglobulinemia consistent with today’s definition of AIH.1
With a global prevalence of 5-20 per 100,000, AIH is uncommon.2 While the disorder affects all age groups and ethnicities, it has a strong female predominance (F:M ratio 3.6:1).2,3 Patients often present with protean symptoms such as general fatigue, appetite loss, and lethargy.2 However, some patients can present with symptoms related to cholestasis and jaundice.
Disease onset can occur in one of three patterns. Approximately 55% of patients present acutely (over days to weeks), 35% have gradual symptom onset (over several months), and 10% are asymptomatic and present with an incidental elevation of liver transaminases.2 At laboratory evaluation, patients have elevated liver transaminases and serum levels of immunoglobulin G (IgG), as well as the autoantibodies ANA, anti-SMA, anti-LKM1, and/or anti-LC1.1,2
As AIH is a diagnosis of exclusion, other, more common causes of hepatitis should be eliminated. The diagnostic criteria include abnormal laboratory tests, periportal hepatitis on histology, and the absence of a viral cause of hepatitis (Table).2 While liver biopsy is the most important diagnostic tool, histopathologic findings in AIH are nonspecific, with no pathognomonic lesions. Thus, the disorder can be mistaken for the other types of hepatitis.4 AIH is characterized by infiltrative mononuclear cells, interface hepatitis, necrosis and fibrosis.4 Fibrosis is present in most patients; Tucker, et al, described the presence of characteristic hyaline droplets in Kupffer cells on hematoxylin and eosin stains of pediatric AIH patients.5 In general, pathological correlations via liver biopsy along with a detailed clinical history are necessary to correctly diagnose AIH.
The literature on AIH imaging is limited, and there are no specific radiologic features of the disorder. On ultrasound, the hepatic echotexture is often coarsened and porta hepatis lymph nodes are enlarged.3 On CT and MRI, the liver has been described as having a heterogeneous appearance, depending on the degree of inflammation and fibrosis.6 Sahni, et al, noted the most common appearance in AIH was surface nodularity in CT and MRI images.6 The presence of ascites on CT scans has also been shown to have significant positive correlations with the fibrotic stage.6 Liver stiffness (whether measured with MRI or ultrasound) may be useful in predicting liver fibrosis, disease severity, and disease activity.3,7
Biliary imaging (either endoscopic cholangiography or MRCP) is important to help diagnose AIH and to distinguish it from other potential causes of cryptogenic cirrhosis; eg, primary sclerosing cholangitis (PSC) or primary biliary cirrhosis (PBC), or to identify an overlap syndrome.7 Overlap syndrome describes variant forms of AIH that present with features of either PSC or PBC. AIH-PSC overlap syndrome is predominantly found in children and young adults, with an incidence of 6-11% of patients with AIH.7AIH-PSC overlap syndrome is identified at cholangiography with irregular bile ducts showing areas of stricture and dilation.7 However, one study showed that irregular bile ducts attributed to architectural distortion from hepatic fibrosis are present in up to 25% of patients with isolated AIH.7
Untreated, AIH is a progressive disease that leads to death in up to 90% of patients by 10 years from diagnosis.8 Immunosuppression is the mainstay of treatment. Patients are first treated with prednisone, followed by azathioprine.2 Appropriate medical management substantially improves prognosis, with a 10-year survival rate of up to 80%.2 Approximately 10% of patients continue to have disease progression despite medical therapy. These patients are treated with liver transplantation. Currently, 4-6% of all pediatric liver transplants are performed for patients with AIH.8 Most patients undergoing liver transplant do well.
However, despite the reported successes, AIH recurs after transplantation in 16 to 43% of patients.7 Treatment of an AIH overlap syndrome involves identification and therapy consistent with the predominant disorder. Patients with AIH-PSC are more likely to die of liver failure and require liver transplantation more often compared to patients with AIH alone.7 Our patient was started on prednisone and continues to be followed. Because there were no changes of PSC at biopsy, our patient is being treated as if she has isolated AIH even though mild duct irregularities appeared on MRCP.
CONCLUSION
Autoimmune hepatitis is an uncommon disease that, left untreated, can lead to hepatic fibrosis, liver failure, and death. Liver biopsy, the preferred method of diagnosis, is characterized by infiltrative mononuclear cells and interphase hepatitis. Imaging is used to help identify changes in fibrosis and cirrhosis and to exclude other causes of cryptogenic cirrhosis.
REFERENCES
- Mackay IR. Historical reflections on autoimmune hepatitis. World J Gastroenterol. 2008;14(21):3292-3300. doi:10.3748/wjg.14.3292
- Mataya L, Patel N, Azzam RK. Autoimmune Liver Diseases in Children. Pediatric Annals; Thorofare. 2018;47(11):452-457. doi:http://dx.doi.org.proxy.library.ohio.edu/10.3928/19382359-20181022-02
- Dong Y, Potthoff A, Klinger C, Barreiros AP, Pietrawski D, Dietrich CF. Ultrasound findings in autoimmune hepatitis. World J Gastroenterol. 2018;24(15):1583-1590. doi:10.3748/wjg.v24. i15.1583
- Tiniakos DG, Brain JG, Bury YA. Role of Histopathology in Autoimmune Hepatitis. Dig Dis. 2015;33 Suppl 2:53-64. doi:10.1159/000440747
- Tucker SM, Jonas MM, Perez-atayde AR. Hyaline Droplets in Kupffer Cells: A Novel Diagnostic Clue for Autoimmune Hepatitis. The American Journal of Surgical Pathology. 2015;39(6):772-778. doi:10.1097/PAS.0000000000000395
- Sahni VA, Raghunathan G, Mearadji B, et al. Autoimmune hepatitis: CT and MR imaging features with histopathological correlation. Abdom Imaging. 2010;35(1):75-84. doi:10.1007/s00261-008-9485-4
- Malik N, Venkatesh SK. Imaging of autoimmune hepatitis and overlap syndromes. Abdominal Radiology. 2017;42. doi:10.1007/s00261-016-1019-x
- Venick RS, Farmer DG, Soto JR, et al. One Thousand Pediatric Liver Transplants During Thirty Years: Lessons Learned. Journal of the American College of Surgeons. 2018;226(4):355-366. doi:10.1016/j.jamcollsurg.2017.12.042
- Hennes EM, Zeniya M, Czaja AJ, et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008;48(1):169-176. doi:10.1002/hep.22322
Affiliations: Ohio University Heritage College of Osteopathic Medicine (Dr Saeed); Phoenix Children’s Hospital (Dr R Towbin); Cincinnati Children’s Hospital and University of Cincinnati College of Medicine (Dr A Towbin).
