Imaging of the brachial plexus
Images





Dr. Lury is a Clinical Assistant Professor of Radiology and Dr. Castillo is a Professor of Radiology and Section Chief of Neurology in the Department of Radiology, University of North Carolina School of Medicine, Chapel Hill, NC.
Most patients with brachial plexopathies complain of vague ipsilateral and nonspecific symptoms. Trauma is the most common cause of brachial plexopathy; tumors are the next most common cause. Infection of the brachial plexus (BP) is rare and may occur after lung disease, such as fungal infection or tuberculosis, or after surgery or trauma. 1 Viral brachial plexitis is rare, and postviral inflammatory processes are also known to affect the BP. Both are self-limiting processes and usually resolve 6 to 12 weeks after their onset. A plexopathy may also arise as a consequence of drug allergy. The heredo-familial form of brachial plexopathy is rare and is seen mostly in men. Postradiation plexopathy is more often seen in patients receiving >6000 cGy. 2
Imaging scheme
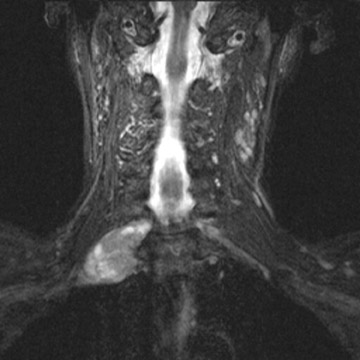
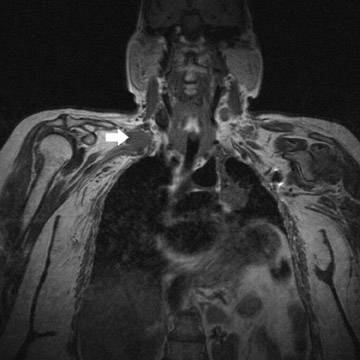
At our institution, magnetic resonance (MR) is the preferred modality for imaging of the BP. 1 To image the BP, we use a large field-of-view (to include both shoulders) and obtain T1-weighted coronal, T1-weighted axial, and T2-weighted axial images (Figure 1A). Using a small field-of-view, we obtain parasagittal T1-weighted images of each BP (Figure 1B). After contrast is given, we repeat the coronal and axial T1weighted images. Fat suppression is recommended for T1-weighted images after contrast administration and is helpful when evaluating certain masses, such as lipomas, in the vicinity of the BP (Figure 2). Fat-suppressed images are also very helpful to evaluate for trauma of the BP. In these images, the injured BP is generally of high signal.
On sagittal views of the BP, we generally include the cervical spine because disc herniations occasionally result in symptoms mimicking a plexopathy. The cervical rib syndrome may also result in ipsilateral brachial plexopathy. 1 It is associated with the presence of an extra rib (cervical rib) and is more common in women. When suspected, the presence of the extra rib may be confirmed by the use of radiographs. This syndrome tends to be unilateral, but bilateral symptoms are occasionally found.
Anatomy
The components of the BP may be recalled by using the following pneumonic: Radiology (roots) technologists (trunks) drink (divisions) cold (cords) beverages (branches). Although classical anatomy uses the above components, imaging anatomy is greatly simplified (Table 1).
The imaging anatomy scheme uses easily identifiable landmarks (such as the anterior and middle scalene muscles and subclavian artery) to divide the BP. 1 The innervation provided by the brachial plexus is reviewed in Table 2. 1
Clinical applications
Trauma
Most traumatic avulsions are seen in newborns (generally due to shoulder dystocia at vaginal delivery) and in young adults (particularly after motorcycle accidents). 3 Erb's palsy, involving avulsion of C5-6, comprises 80% to 90% of brachial plexopathies in the newborn. 4 In this palsy, the affected arm is internally rotated and adducted, the elbow extended, the forearm pronated, and the wrist is flexed. Complete recovery can occur but may take months. All supraganglionic avulsions have a poor prognosis. Dejerine-Klumpke palsy is rare, comprising only 1% of all brachial plexopathies in the newborn. 5 In these patients, the elbow is flexed, the forearm is supinated, the wrist is extended, and there is claw-like deformity of the hand. The muscles in the involved arm are weak and Horner's syndrome may be present. Resolution of this plexopathy is possible. The third type of brachial plexopathy in the newborn (accounting for approximately 10% of cases) is a complete avulsion of the BP, resulting in absolute weakness and lack of muscle control and tone. 3 There is no treatment for this type of injury, and there is no recovery. In about 10% of all neonatal brachial plexopathies, the involvement is bilateral. Injury to the BP may also occur if one arm is kept in an awkward position for prolonged periods of time. 6
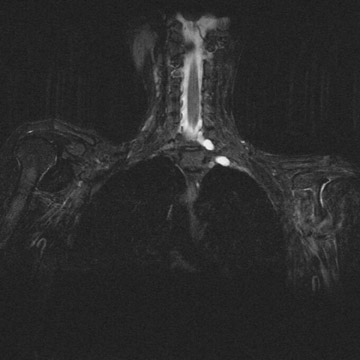
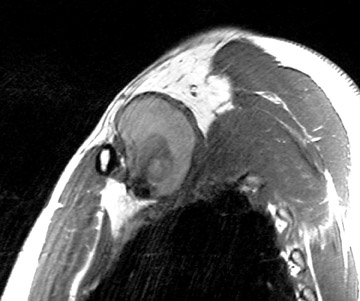
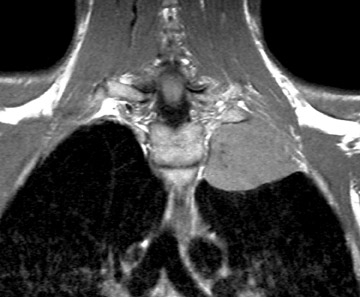
Avulsion of the BP at its spinal cord origin results in formation of intraspinal or extraspinal cerebrospinal fluid collections and/or hematomas. 1 Pseudo-meningoceles will appear in 80% of patients with avulsions, but not all of these will fill with contrast at myelography. 7 The sensitivity and specificity of postmyelogram computed tomography (CT) are 73% to 83% and 87% to 100%, respectively, in avulsions of BP (because of the lack of filling of the pseudomeningoceles, which is the most important CTfinding in avulsion). 8 Thus, MR is a better imaging method for detecting avulsion of the BP than is postmyelogram CT. MR myelography is helpful in identifying pseudomeningoceles 9 (Figure 3). Establishing the site of injury will help decide the mode of treatment. 10-12 For supraganglionic avulsions, there generally is no treatment, whereas intraganglionic or distal avulsions may undergo microsurgical re-anastomosis and/or grafting. Some supraganglionic avulsions may be treated by microsurgical anastomosis. Most of these patients will not recover any significant function, but the procedure will decrease their pain. Hematomas in the vicinity of the BP may require decompression to avoid pressure necrosis of the nerves, and subclavian artery aneurysms and pseudoaneurysms may need to be clipped, occluded, or stented (Figure 4). Chronic injuries manifest as atrophy and gliosis of the spinal cord at the level of the avulsion.
Tumor
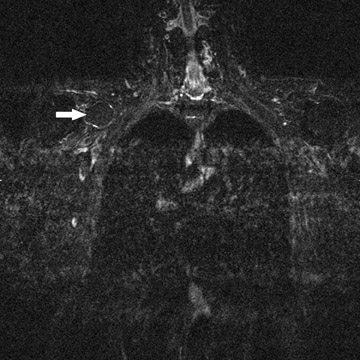
Sensory symptoms are seen mostly in adults and may occur after radiation or indicate the presence of a tumor. 13 In postirradiation plexopathy, the nerves are enlarged diffusely and typically appear as high signal on T2-weighted sequences (Figure 5). The BP may also show some enhancement after gadolinium administration. 2 Tumors commonly produce both motor and sensory symptoms. Patients with both a BP palsy and Brown-Séquard's syndrome usually have an injury at the level of the root entry zone into the cord. Involvement of the phrenic nerve and scapular winging indicate an injury to the supraclavicular BP. A BP palsy with Horner's syndrome indicates an injury to the infraclavicular segment.
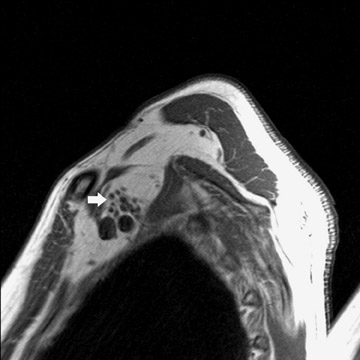
Primary tumors occur in younger patients and may be nerve-related (schwannoma/neurofibroma) or sarcomas 14 (Figure 6). Benign tumors are generally well-demarcated and enhance variably. Sarcomas may be either well-demarcated or infiltrative. Secondary tumors are generally seen in older patients and include lung cancer (Pancoast's tumor) and metastases (commonly from primary breast cancer) (Figures 7 and 8). In patients with early Pancoast's tumor, the only clue to the presence of a lesion may be a lesion of intermediate signal intensity effacing the normal bright T1 appearance of the triangular region of fat located superior to the lung apex, medial to the scalene muscles and lateral to the spine. Larger tumors are easier to identify. In all of these tumors, multiplanar imaging is necessary to exclude invasion of the BP, which may preclude surgery.
Occasionally, lymphoma and leu-kemia (including chloromas) may also involve the BP. These tumors are generally ill-defined and infiltrative and enhance after gadolinium is administered. Benign masses may result in symptoms by virtue of compression of the BP, whereas malignant ones compress, infiltrate, and destroy it.
Imaging also plays a role in treating chronic pain associated with BP pathology. This may be treated by ablation of the plexus, which is generally done by injecting alcohol into the proximal aspect (trunks) of the plexus. The trunks are localized by CT in between the anterior and mid/posterior scalene muscles. The lysing material is combined with iodinated contrast so that its distribution can be tracked with CT.
Conclusion
Brachial plexopathy is most commonly the result of trauma or tumor. Imaging with MR yields important information regarding etiology and the specific location of pathology, and can aid in directing possible therapy.