Heterotaxy syndrome with polysplenia
Images


Case Summary
The patient was a 7-year-old female who presented to the emergency department with a one-day history of abdominal pain and emesis. Her medical history was not provided at the time of imaging request. The patient was found to have an elevated white count. Standard chest films and computed tomography (CT) of the abdomen were requested to rule out appendicitis.
Findings
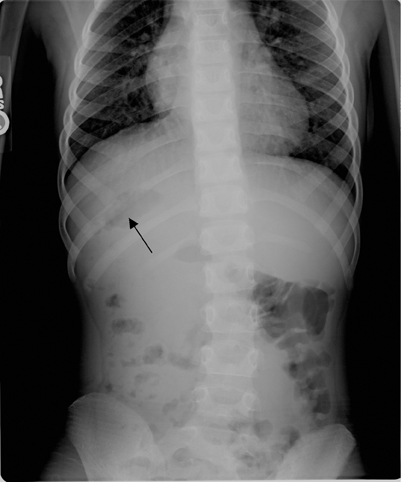
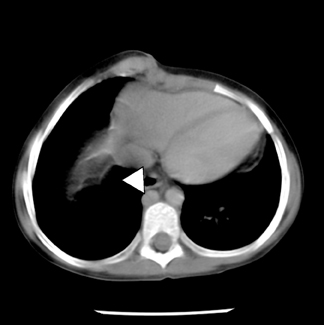
There was no evidence of acute infiltrate on front (PA) or lateral chest films, which showed mild cardiomegaly; bilateral morphologically left main stem bronchii (Figure 1). Abdominal and pelvic CT revealed polysplenia, midline liver, situs ambiguous, and interrupted inferior vena cava with azygous continuation (Figures 2 and 3).
Diagnosis
Heterotaxy syndrome with polysplenia
Discussion
Heterotaxy syndrome is a general term that describes disruption in normal positioning of the visceral organs in the chest and abdomen. This generality encompasses the wide spectrum of findings found with this disorder. The arrangement of visceral organs and vessels, which otherwise follow a standard developmental pattern, is abnormal. In situs solitus, the heart apex, spleen, stomach, aorta, and bi-lobed lung lay to the left of midline; the tri-lobed lung, gallbladder, liver, and inferior vena cava lay to the right. In situs inversus, these organs are located the exact opposite of the normal asymmetry. Both situs inversus and situs solitus are orderly arrangements of the viscerovascular structures of the body that are delineated during embryogenesis. In situs ambiguous, otherwise known as heterotaxy syndrome, the arrangement of organs within the body is disorderly. The prevalence is estimated to be 1.4 in 10,000 infants. This is likely an underestimation, as it is based on patients with clinical manifestations of heart disease.1
Patients with situs ambiguous traditionally have been categorized based on the number of spleens. Those with polysplenia typically are associated with hyparterial pulmonary bronchi, while asplenic patients usually have eparterial bronchi. Several overlapping anatomical abnormalities are found in both of these entities. Certain cases do not fit into this classification.2 Nonetheless, the traditional system will be utilized to characterize the findings in this case.
Asplenic patients have a higher incidence of congenital heart disease with serious cardiac manifestations.2,3 This typically leads to earlier presentation and detection. In contrast, there have been reports, as in this case, of asymptomatic patients with polysplenia diagnosed later in life.4 While cardiac defects are comparatively fewer in this group, the diagnosis carries a mortality rate of 75% at 5 years of age.5
Cardiac anomalies in the heterotaxy syndrome occur during embryogenesis. Common morphologic abnormalities include atrial septal defects, ventricular septal defects, and bilateral superior vena cava. In polysplenia patients, the inferior vena cava is commonly discontinuous with the atrium. Venous return is via the left-sided azygous or occasionally hemi-azygous vessels, as seen in this case. In comparison, the asplenic grouping usually has normal venous drainage via the IVC. However, abnormal venous drainage above the diaphragm in the form of TAPVR is a frequent finding in asplenia. Other vessel abnormalities include transposition of the great arteries.2,3,5 Visceral positioning and heart morphology are not always congruent.3
Other manifestations associated with the polysplenic group include bilateral bi-lobed lungs, a midline liver, variable stomach location, and hyparterial bronchi.2,5 Intestinal malrotation is common in this syndrome, but complications such as obstruction or volvulus are infrequent.6 Other less common anatomic variations are biliary atresia, pancreatic malformations, and urogenital anomalies.2,5
In asplenia, findings typically include bilateral tri-lobed lungs, eparterial bronchii and, occasionally, ipsilateral location of the aorta and inferior vena cava. Gastrointestinal abnormalities are also frequently found in this subset.2,3
Heterotaxy syndrome’s etiology is not yet known. However, altered embryogenesis via a combination of several internal and external influences is thought to contribute to the abnormal asymmetrical anatomic patterning. Animal models have delineated certain chromosomal and genetic foci also thought to be involved with this sequencing.7 A familial distribution, specifically X-linked recessive and autosomal recessive modes of inheritance, have been reported, but most cases are sporadic in nature.7,8
Treatment depends on the associated abnormalities. Prognosis is generally poor in those affected with cardiac abnormalities. Improvements in antenatal diagnosis, and corrective measures such as the Fontan procedure, have significantly decreased the morbidity and mortality in patients that are candidates for this type of treatment.9 Functionality of the spleen should be assessed if splenic abnormalities are present. Patients with nonfunctional spleens or asplenia are at an increased risk for infections from encapsulated organisms, which can lead to septicemia and death. Typically, treatment consists of prophylactic antibiotics and immunizations.10 Malrotation of the intestinal tract can be surgically treated. One recent report recommends surgery only if symptoms or imaging dictate an obstruction and ischemia is rare.6 The surgeon must be aware of the individual’s specific anatomy as there can be significant variability in each case. This information could have serious implications in management and treatment for the patient.
Conclusion
Heterotaxy syndrome is a rare disorder that commonly presents early in life secondary to associated cardiac manifestations. However, it has many possible presentations due to the variability of organ involvement. Occasionally, it can go undetected for many years, as in this case. Identification of the subtle anatomic manifestations can greatly impact the treatment of primary and secondary sequelae of this syndrome.
- Hernanz-Schulman M. Asplenia/Polysplenia. Available at: http://www.emedicine.com/Radio/topic58.htm. Accessed 2005.
- Ticho BS, Goldstein AM, Van Praagh R. Extracardiac anomalies in the heterotaxy syndromes with focus on anomalies of midline-associated structures. Am J Cardiol. 2000;85:729-734.
- Applegate KE, Goske MJ, Pierce G, Murphy, D. Situs revisited: Imaging of the heterotaxy syndrome. Radiographics. 1999;19:837-852.
- Marx MV, Van Allan R. SIR 2005 film panel case: Heterotaxia with polysplenia. J Vasc Interv Radiol. 2005;16:1055-1059.
- Peoples WM, Moller JH, Edwards JE. Polysplenia: A review of 146 cases. Pediatr Cardiol. 1983;4:129-137.
- Choi M, Borenstein SH, Hornberger L, Langer JC. Heterotaxia syndrome: The role of screening for intestinal rotation abnormalities. Arch Dis Child. 2005;90:813-815.
- Belmont JW, Mohapatra B, Towbin JA, Ware SM. Molecular genetics of heterotaxy syndromes. Curr Opin Cardiol. 2004;19(3):216-220.
- Lin AE, Ticho BS, Houde K, et al. Heterotaxy: Associated conditions and hospital-based prevalence in newborns. Genet Med. 2000;2:157-172.
- Kaulitz R, Hofbeck M. Current treatment and prognosis in children with functionally univentricular hearts. Arch Dis Child. 2005;90:757-762.
- Long S, Pickering L, Prober C. Principles and Practice of Pediatric Infectious Diseases, 2nd Edition. Churchill Livingstone. 2003:651-652; An imprint of Elsevier.