Benign solitary fibrous tumor originating from the parietal pleura
Images

Case Summary
A 64-year-old Asian man reported dyspnea on exertion over the prior few weeks, which was progressively getting worse. The patient had a right-sided thoracentesis a year previously at an outside hospital and was told that he had a "spot" in his right lung. Upon examination, he was afebrile and his oxygen saturation was 74% on room air. Physical examination was positive for digital clubbing, and auscultation of the right lung revealed a complete lack of breath sounds. The patient admitted to a 50-pack/year smoking history prior to quitting 20 years previously but denied any weight loss or night sweats. Complete blood count and basic metabolic panel were within normal limits.
Diagnosis
Benign solitary fibrous tumor originating from the parietal pleura.
Imaging Findings
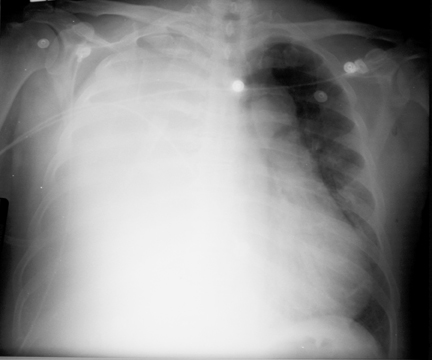
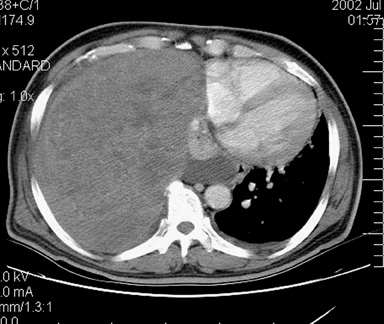
Upon admission into the emergency department, chest X-ray revealed complete opacification of the right hemithorax with mediastinal shift to the left (Figure 1). An attempt at thoracentesis was unsuccessful for the retrieval of fiuid. A subsequent contrast-enhanced chest computedtomography (CT) scan revealed a very large, well-encapsulated, heterogeneous mass in the right hemithorax that was compressing the right main stembronchus and pushing the mediastinum to the left (Figure 2). CT also showed an associated right pleural effusion. Radiographically, solitary fibrous tumors of the pleura (SFTP) tend to appear as well-demarcated, solitary, enhancing masses that form obtuse angles with the chest wall or mediastinum. They are more often found in the middle and lower aspects of the chest. Calicifications (~5%) and pleural effusions (~8% to17%) are uncommon. 1
A multiplanar, multisequence contrast-enhanced magnetic resonance image (MRI) was obtained, confirming the findings of the chest CT. In addition,there was no evidence of invasion of the chest wall (Figure 3). Solitary fibrous tumors of the pleura usually exhibit low signal characteristics on T1- and T2-weighted images (T2WI), indicative of fibrosis. However, high signal on T2WI can represent areas of necrosis or hemorrhage. 2
Case Follow-Up
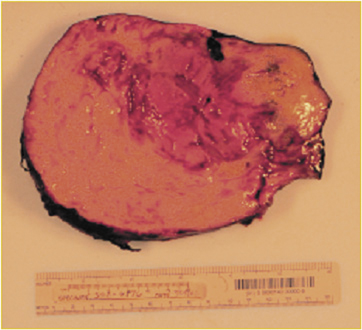
The imaging findings warranted a biopsy and surgical resection (Figure 4). The patient was brought to the operating room and underwent resection of the tumor and wedge resection of the right middle and right lower lobes. The mass was adherent to the chest wall, without any evidence of mediastinal invasion.
Discussion
Solitary fibrous tumors of the pleura are very rare,slowly growing tumors and represent <5% of alltumors involving the pleura. 3-5 As of 2001, approximately 600 cases had been reported in the literature. 6 Solitary fibrous tumors of the pleura generally occur in patients >50 years of age. One study conducted over an 18-year period at Memorial Sloan-Kettering Cancer Center (MSKCC) found a positive association between malignancy and a tumor size >10 cm. 7
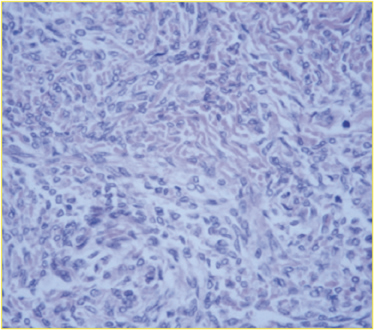
In the past, there was some mystery as to the histiogenesis of SFTP. It was thought that these tumors were related to mesotheliomas. Also, at one time, SFTPs were called by different names, such as benign or localized mesothelioma, benign fibrous mesothelioma, and subpleural fibroma. 5 However, they have no established relationship to asbestos exposure or smoking, and their origin has been revealed as submesothelial mesenchymal cells (presence of fibroblasts with negative staining with cyto-keratin). 8 Solitary fibrous tumors of the pleura originate from either the visceral or parietal pleura; the former are more common. Most (>80%) SFTPs are benign. However, both benign and malignant types should be completely excised because of their growth potential. Malignant SFTPs have a greater chance of local recurrence and metastasis. If not completely excised, the malignant form may recur years after excision, whether the original SFTP was benign or malignant. Solitary fibrous tumors of the pleura have rarely been known to metastasize.
Malignant tumors include at least one of the following characteristics 9 : 1) High mitotic count [>4 mitosis/10 HPF (×400)]; 2) presence of a large area of necrosis; 3) nuclear crowding and overlapping; and 4) nuclear atypia. The number of mitoses tends to be the best indicator of malignancy. 10 The best prognostic factors are encapsulation, pedunculation, and resectability. 11
Solitary fibrous tumors of the pleura have no gender predilection and are often incidental findings on chest X-ray. However, patients can become symptomatic, presenting with chest pain, dyspnea, cough, hypertrophic osteoarthropathy, digital clubbing, and hypoglycemia. There is no relationship between the size of the tumor and the presence of hypertrophic osteoarthropathy and digital clubbing. Hypoglycemia occurs because SFTPs may secrete insulin-like proteins. 1 Solitary fibrous tumors may also arise in the pericardium, mediastinum, pancreas, or paranasal sinuses. 12
Since no current imaging modality can distinguish between the benign and malignant forms, biopsy is indicated. Often the biopsy will be inconclusive, revealing only disorganized spindle cells. 4 When adequate samples are obtained, they stain positive for 12,13 and negative for cytokeratin. Since imaging studies and biopsies are usually equivocal for the presence of malignancy, every suspected SFTP should be surgically removed.
Conclusion
Solitary fibrous tumors of the pleura are slow-growing tumors that are not histologically related to mesotheliomas. Most of these tumors are benign, but regardless of their categorization, total surgical excision is indicated and likely diagnostic. Complete resection is the best prognostic factor. 10 Those who have undergone surgery should receive yearly follow-up CT scans to rule out recurrence. For most, recurrence does not occur (regardless of histologic classification), and surgical excision is curative. However, recurrence can occur from either a benign or malignant initial SFTP. Neither postoperative chemotherapy nor radiotherapy has been shown to be required.
What makes this case of SFTP even more rare is its benign diagnosis as such a large tumor (>>10 cm), its parietal pleural basis, and the presence of a pleural effusion.