CHARGE Syndrome
Case Summary
A neonate was transferred to our neonatal intensive care unit (NICU) with respiratory failure. The child had been born at 39 weeks’ gestation with a nuchal cord and required intubation at birth. The mother’s reported pregnancy history was unremarkable, and no antenatal imaging was available. Upon transfer to the NICU, the patient was found to have a large patent ductus arteriosus, hyperphosphatemia, hypocalcemia, conductive hearing loss, and dysmorphic facial features. Hematologic workup revealed severe combined immunodeficiency. Physical exam was positive for dysmorphic facial features, including ear anomalies and micropenis.
Chromosomal microarray (CMA) analysis was unrevealing, but whole-exome sequencing confirmed a de novo chromodomain helicase DNA-binding protein 7 (CHD7) splice-site variant (c.2498+5 G>A).
The patient was discharged home tracheostomy- and feeding tube-dependent after an 8.5-month hospitalization on prophylactic antimicrobials (acyclovir, azithromycin, fluconazole, and trimethoprim-sulfamethoxazole) and infusion of intravenous immunoglobulins. The patient returned to the hospital at 10 months of age, after having increased diarrhea and vomiting, followed by left-arm rigidity and right-eye deviation.
As of the end of the first year of life, the patient was awaiting a thymic transplant. The patient has been readmitted multiple times for infections.
Image Findings
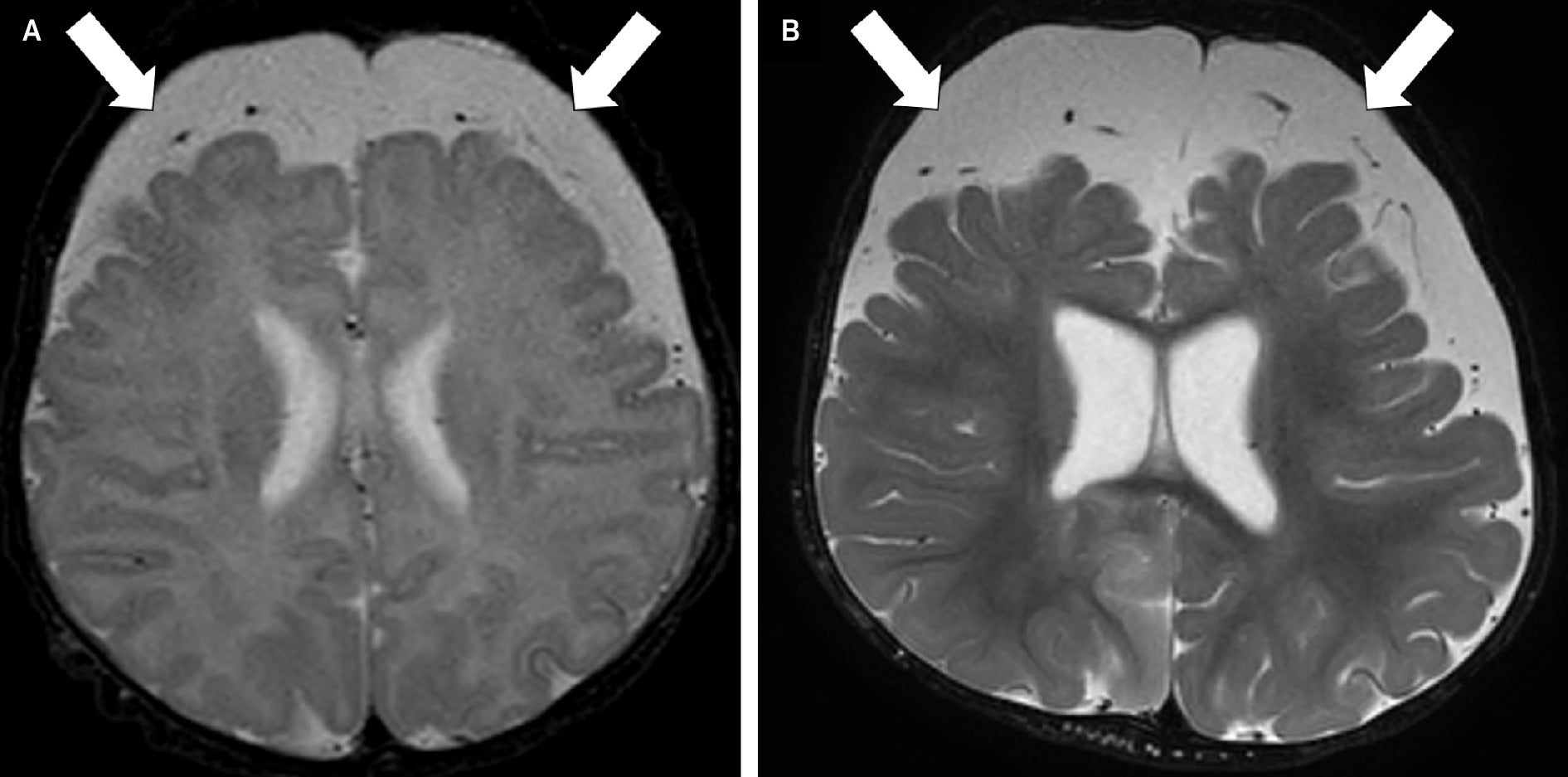
Chest x-ray at initial presentation revealed an absent thymic shadow. Brain MRI at 22 days of age showed frontal-predominant low parenchymal volume ( Figure 1A ), which persisted at 10 months ( Figure 1B ). CT revealed lack of the clivus ( Figure 2 ). Though dedicated imaging of the temporal bones was not performed, semicircular canals were not seen on CT of the head. There was no choanal atresia, and globe contours were normal.
Axial T2-weighted MRI of the brain obtained at 22 days of age (A) and 10 months (B) demonstrates low parenchymal volume, most pronounced in the frontal lobes, with expanded frontal extra-axial cerebrospinal fluid (arrows). Synthetic MRI at 10 months of age revealed brain parenchymal fraction of 10.3 standard deviations below normal for age, CSF volume 6.7 standard deviations above normal for age, and intracranial volume 3.9 standard deviations below normal for age.
Sagittal CT of the head acquired at 10 months of age uncovered the lack of a clivus (arrow).

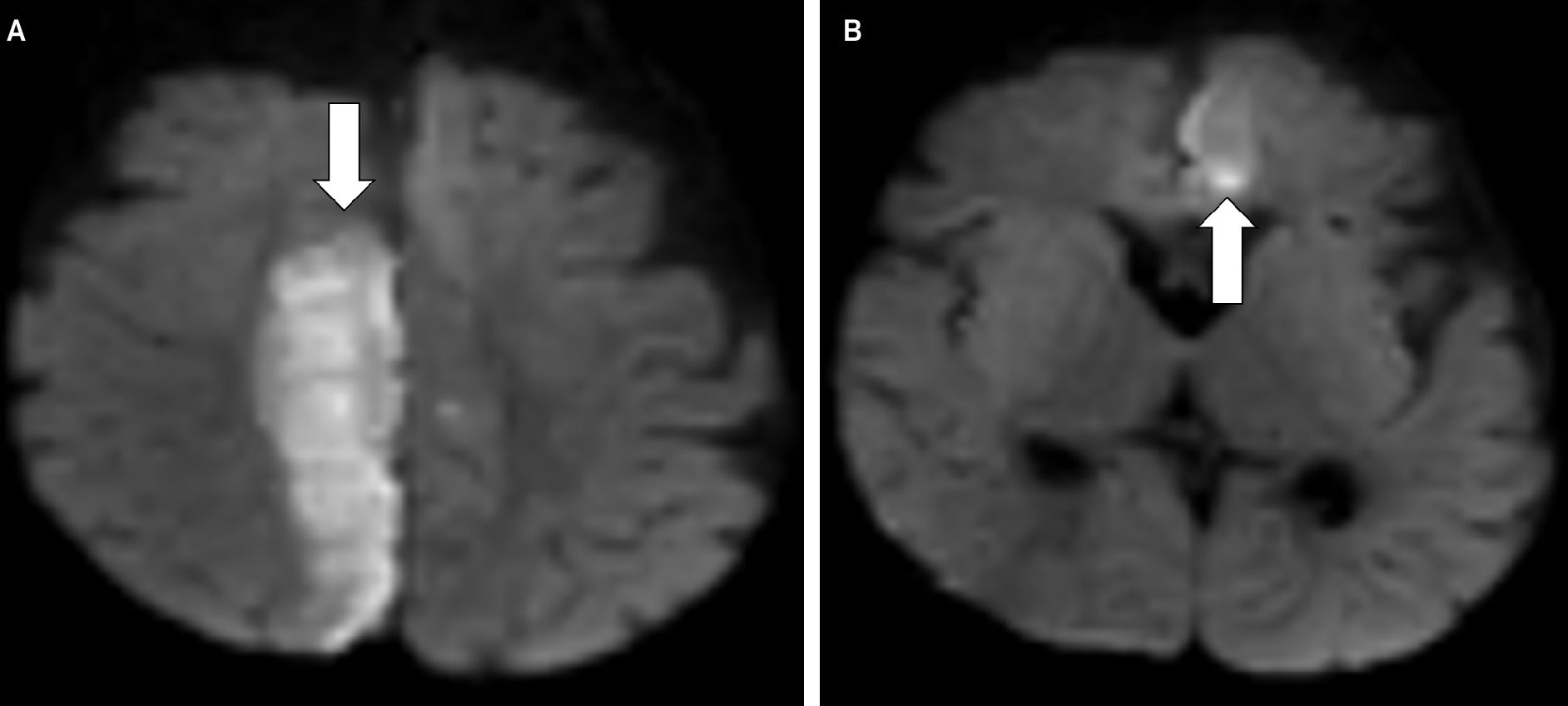
MRI performed at 10 months of age showed multifocal diffusion restriction corresponding to multiple vascular territories ( Figure 3 ). magnetic resonance angiography and magnetic resonance venography showed no focal stenosis in any of the major branches of the Circle of Willis and no dural sinus thrombosis.
Axial diffusion-weighted MRI of the brain exhibits acute ischemia (arrows) in the posterior right paramedian frontal and parietal lobes (A) and the anterior left frontal lobe (B).
Diagnosis
CHARGE syndrome.
The differential diagnosis includes benign enlargement of the extra-axial spaces, which typically presents with macrocephaly; normal variation of the thymic shadow, although the final diagnosis supported athymia; and isolated clival hypoplasia.
Discussion
CHARGE syndrome is a rare, autosomal-dominant genetic disorder that affects multiple areas of the body.1 The name “CHARGE” is an acronym for several common features of the disorder, including coloboma, heart defects, atresia of the choanae (also known as choanal atresia), growth retardation, genital abnormalities, and ear abnormalities. In approximately 60%-65% of cases, the syndrome is caused by heterozygous loss‐of‐function mutations in the CHD7 gene, a chromatin remodeler gene essential for normal development.2, 3
The prevalence of CHARGE syndrome is approximately 1 in 10,000 births, and it is not typically inherited, with most cases being sporadic.4 Individuals with CHARGE syndrome may also have distinctive facial features, cognitive function ranging from normal intelligence to major learning disabilities, and various other health problems affecting the kidneys, immune system, spine, and limbs. CHARGE was originally based on the clinical presentation of 4-6 cardinal signs. It has since been updated by Blake et al, who focused on brainstem and cranial nerve anomalies, and Verloes, who focused on the 3C triad (coloboma, choanal atresia, abnormal semicircular canals), which is highly predictive of a CHD7 mutation.4, 5 CMA is initially performed for infants with multiple anomalies.6 However, if CMA is nondiagnostic, then CHD7 genetic testing is recommended in potentially affected individuals.
The CHD7 gene plays a crucial role in brain development, and heterozygous mutations in this gene have been characterized by brain structural anomalies and associated with various neurological conditions like CHARGE syndrome.7 An ATP-dependent chromatin remodeler, CHD7 is essential for the development of migratory, multipotent neural crest cells by controlling gene expression. Studies have shown that CHD7 is indispensable for mammalian brain development and controls a core neuronal differentiation program during cerebellar development.8 One study utilizing MRI and high-angular resolution diffusion MRI tractography demonstrated statistically significant reduction in volume of the bilateral putamen, brainstem, bilateral cerebellum, bilateral globus pallidus, and left subthalamic nucleus in patients with CHARGE syndrome compared with their gender- and age-matched controls.9
Thymic aplasia and hypoplasia are observed in patients with CHD7 mutations.10 In mouse embryos, Randall et al reported that approximately 11% of mice with the heterozygous CHD7 mutation had either thymic hypoplasia or an ectopic thymus, which was correlated with downregulation of the FOXN1 gene.10
As part of his stroke workup, our patient was found to have a patent foramen ovale with shunting that puts him at risk of thromboembolic events, especially given the multifocal nature of the stroke. This could have been precipitated by diarrhea- and/or vomiting-induced dehydration. The patient has been referred to the cardiology service for device closure.
There is no known increased stroke risk in CHARGE syndrome. The patient’s stroke could have been precipitated by diarrhea and/or vomiting induced dehydration, which was not specific to the patient’s diagnosis of CHARGE.
Conclusion
This case highlights a unique case of CHARGE with a CHD7 variant in which the diagnosis was not immediately evident on imaging of the head as there was no choanal atresia and the globes appeared normal. Absence of a thymic shadow early in life may aid in suggesting this disorder. Clival hypoplasia may be a previously unreported but related finding. Although low parenchymal volume is nonspecific, frontal predominance may provide an additional diagnostic clue.
References
Citation
Wieland, J, Wieland, D, Estiphan T, Weakley, B, Weakley D, Mangum T, Knoll J, Pfeifer CM. CHARGE Syndrome. Appl Radiol. 2025;(4):.
doi:10.37549/AR-D-25-0107
September 23, 2025