Clinical Applications of Gadopiclenol in Cardiac MRI
CE credits are available for this article here.
Introduction
Cardiac magnetic resonance imaging (MRI) is a well-established, noninvasive tool that provides high-quality assessments of cardiac structure and function, without the ionizing radiation required by other techniques such as cardiac catheterization and contrast-enhanced computed tomography.1 In cardiac MRI, three-dimensional image acquisition techniques help identify congenital anomalies and evaluate right ventricular anatomy.1,2 Cine MR sequences, typically acquired using steady-state free precession and played in movie mode, can assess ventricular function and quantify volumes.2,3 Cardiac MRI is also regarded as the ‘gold standard’ for evaluating global and regional left ventricular size and function.2,3 In the setting of valvular heart disease, cardiac MRI can assess both valve morphology and function, in addition to ventricular response.3–5 This modality also offers an advantage over echocardiography in patients with poor acoustic windows due to body size or lung disease.3 Finally, coronary MR angiography leverages the high signal of coronary blood flow to enhance contrast between the vessels and surrounding myocardium, allowing for noninvasive assessment of coronary artery anatomy and potential disease.2,3
The introduction of gadolinium-based contrast agents (GBCAs) has further driven the diagnostic capabilities of cardiac MRI by increasing the sensitivity and specificity for detecting a broad range of pathologies.6 Although considered safe, cases of nephrogenic systemic fibrosis (NSF) in patients with severe renal insufficiency and the potential for gadolinium retention in body tissues have prompted the development of GBCAs with improved physicochemical properties.7 Gadopiclenol, the most recent GBCA to be approved by the US Food and Drug Administration, offers high relaxivity and kinetic stability, which enables the use of half the gadolinium dose of standard GBCAs.8,9 This article discusses the clinical applications and value of cardiac MRI, as well as the role of gadopiclenol in improving patient care.
The Clinical Value of Gadopiclenol in Cardiac Imaging
All GBCAs contain gadolinium (Gd3+), a paramagnetic ion that alters the magnetic properties of nearby water molecules to enhance the contrast between normal and pathological tissues on T1-weighted images.7,10 This differentiation is particularly beneficial in cardiac MRI, where it can help detect a wide range of pathologies, including myocarditis, cardiomyopathy, congenital heart diseases, and myocardial viability.2,11–13 Gadolinium enhancement has also demonstrated utility in stress perfusion imaging to better understand myocardial blood flow for the assessment of ischemia and severity of coronary artery disease.2,11,14,15
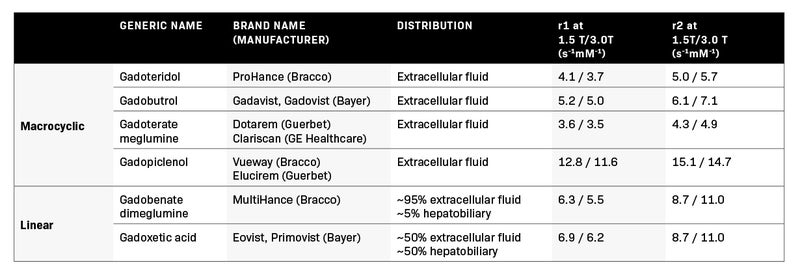
Gadopiclenol is a welcome advancement to the GBCA landscape, owing to its macrocyclic structure, which imparts high kinetic stability and a relaxivity that is 2- to 3-fold higher than that of other standard GBCAs and maintained across different field strengths (Table 1).16–23 Over the past 20 years, numerous randomized controlled trials have confirmed the diagnostic performance of a high- relaxivity GBCA compared with an equivalent dose of a standard-relaxivity agent across many clinical applications.24–30 In similarly designed phase 3 randomized clinical studies, a 0.05 mmol/kg dose of gadopiclenol yielded a diagnostic quality comparable to that of a 0.1 mmol/kg dose of a standard GBCA in terms of the degree of contrast enhancement and quality of morphologic lesion characteristics, suggesting that higher relaxivity enables the administration of a lower gadolinium dose.31,32
Properties of US Food and Drug Administration-Approved Gadolinium-Based Contrast Agents.8,9,16–23
GBCA retention in body organs is influenced in part by kinetic stability, which, owing to their cage-like structure, is inherently higher among macrocyclic agents than linear contrast.33 Although some degree of gadolinium retention has been observed with all GBCAs, the higher kinetic stability of macrocyclic agents results in a lower possibility for Gd3+ ion dissociation, reducing the theoretical risk of NSF development and gadolinium retention in tissues.34 Likewise, studies conducted in rat models demonstrate lower and dose-dependent gadolinium retention with gadopiclenol compared to linear GBCAs.35–37 While no evidence suggesting harmful clinical effects from gadolinium retention has been published,29 the opportunity to lower gadolinium exposure without losing diagnostic quality makes gadopiclenol an appealing contrast option. As clinic experience with gadopiclenol grows, its overall safety profile in adult and pediatric populations is becoming increasingly well established. According to a recent US post-marketing surveillance report based on more than 880,000 administrations of gadopiclenol, no serious adverse events and a very low rate of nonserious adverse events (1 case per every 27,580 exposures) were observed.38 Moreover, the types of adverse events observed were similar to those reported for other GBCAs available for clinical use.38
Experience with Gadopiclenol
At West Virginia University, our practice regularly sees patients with complex cardiovascular conditions for which cardiac MRI often proves to be invaluable, as demonstrated in Figures 1–4.
Case 1: A Man Evaluated for Pericarditis
In the first case, a 29-year-old male patient with a past medical history significant for pericarditis presents to the emergency department with complaints of chest pain, severe in intensity, worse when lying down and improved with sitting. Due to concern about pericarditis, the patient had been treated with non-steroidal anti-inflammatory drugs (NSAIDs; ibuprofen 600 mg three times daily) and colchicine 0.6 mg twice daily, which were prescribed during the previous episode. On presentation, the patient had a low- grade fever of 100.5° F, and the rest of the physical examination was unremarkable.
Blood work, including complete blood count, comprehensive metabolic panel, and troponin, was unremarkable. Elevated C-reactive protein of 130.4 (normal, <8 mg/L) and erythrocyte sedimentation rate of 32 mm/hr (normal, 0-15 mm/hr) were noted. Workup including antinuclear antibody, rheumatoid factor, cyclic citrullinated peptide antibody IgG, anti-double-stranded DNA, and anti-Sjogren’s antibodies (anti-SS-A and SS-B) were negative. C3 and C4 complement levels were normal. An electrocardiogram and chest x-ray were unremarkable. An echocardiogram revealed a small localized pericardial effusion located anterior to the right atrium.
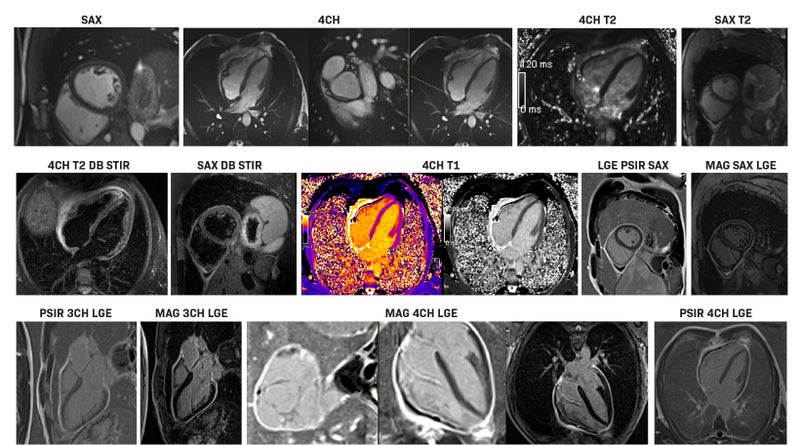
For strong suspicion of pericarditis and given the history of prior pericarditis episodes, a cardiac MRI was performed with 12 mL of gadopiclenol, which revealed a circumferential delayed gadolinium enhancement of the pericardium strongly suggestive of active pericarditis (Figure 1). There was no pericardial thickening (3 mm; however, trace pericardial fluid was noted). Linear myocardial delayed enhancement was noted in the lateral and inferior walls. Cardiac MRI was diagnostic for pericarditis. The patient started treatment with NSAIDs, colchicine, and eventually rilonacept and was discharged after clinical improvement.
Cardiac MRI sequences (enhanced with 12 mL gadopiclenol) in a 29-year-old male patient with a past medical history of pericarditis presenting to the emergency department with complaints of chest pain. He was diagnosed with pericarditis. Abbreviations: 4CH, 4 chamber view; DB STIR, double inversion recovery short tau inversion recovery; LGE, late gadolinium enhancement; MAG, magnitude; PSIR, phase sensitive inversion recovery; SAX, short axis
Case 2: A Woman Evaluated for Cardioverter Defibrillator Implantation for Sudden Cardiac Death Prevention
In a second case, a 65-year-old female patient with a relevant past medical history significant for hypertrophic obstructive cardiomyopathy, left anterior descending bridging, and a family history of sudden cardiac death in a second-degree relative in the seventh decade of life was seen in the electrophysiology clinic for the evaluation of cardioverter defibrillator implantation for sudden cardiac death prevention. An echocardiogram revealed a reverse septal curvature variant with evidence of dynamic left ventricular outflow tract obstruction and a peak outflow tract gradient of 95 mmHg with Valsalva and prominent systolic anterior motion of the mitral valve. Holter monitoring revealed one asymptomatic run of non-sustained ventricular tachycardia lasting 10 beats at a rate of 160 beats per minute.
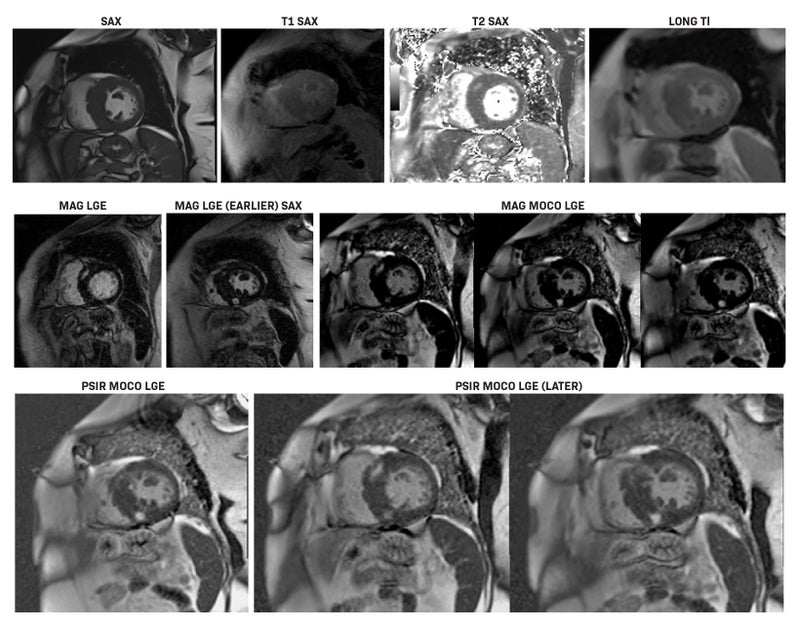
For the quantification of fibrosis burden, a cardiac MRI was performed with 12 mL of gadopiclenol. It revealed globally prolonged native T1 time and extracellular volume (ECV) with localized fibrosis in the superior and inferior right ventricular insertion points (Figure 2). Myocardial fibrosis was quantified at 6.1% (low risk). There was evidence of inferior and anterior extensive right ventricular insertion point fibrosis. The cardiac MRI also confirmed asymmetric septal wall thickening along with a separate myocardial crypt in the mid-anteroseptal segment and flow acceleration in the left ventricular outflow tract due to systolic anterior motion of the mitral valve. Cardiac MRI risk stratification placed the patient at low risk, avoiding the need for an implantable cardioverter defibrillator based on several recent American College of Cardiology/American Heart Association Appropriateness Criteria.39
A 65-year-old female evaluated for cardioverter defibrillator implantation for sudden cardiac death prevention. Cardiac MRI with 12 mL gadopiclenol revealed globally prolonged native T1 time and extracellular volume with localized fibrosis in superior and inferior right ventricular insertion points. Abbreviations: LGE, late gadolinium enhancement; MAG, magnitude; MOCO, motion corrected; PSIR, phase sensitive inversion recovery; SAX, short axis; TI, inversion time.
Case 3: A Patient With Microvascular Obstruction
Cardiac MRI is also helpful in identifying microvascular obstruction, as demonstrated in the case of a 78-year-old male patient with a past medical history of coronary artery disease status post-percutaneous intervention to the mid left anterior descending artery, and medically managed complex right coronary artery disease, type 2 diabetes mellitus, and hyperlipidemia. The patient presented with complaints of progressively worsening exertional chest pain and shortness of breath.
Echocardiography revealed very severe left ventricular systolic dysfunction (LVEF 20%) with global hypokinesis and left ventricular end-diastolic pressure >30 mmHg. For further evaluation, the patient underwent left heart catheterization revealing severe three-vessel coronary artery disease involving critical distal left main (90%), critical ostial left anterior descending (95%) and left circumflex (90%), and chronic total occlusion of right coronary artery (100%). A cardiac MRI was performed for viability assessment using 9.7 mL of gadopiclenol (Figure 3).
Cardiac MRI sequences (enhanced with 9.7 mL gadopiclenol) in a 78-year-old male patient presenting with complaints of progressively worsening exertional chest pain and shortness of breath. He was diagnosed with microvascular obstruction. Abbreviations: 2CH, 2 chamber view; 4CH, 4 chamber view; LGE, late gadolinium enhancement; MAG, magnitude; PSIR, phase sensitive inversion recovery; SAX, short axis.
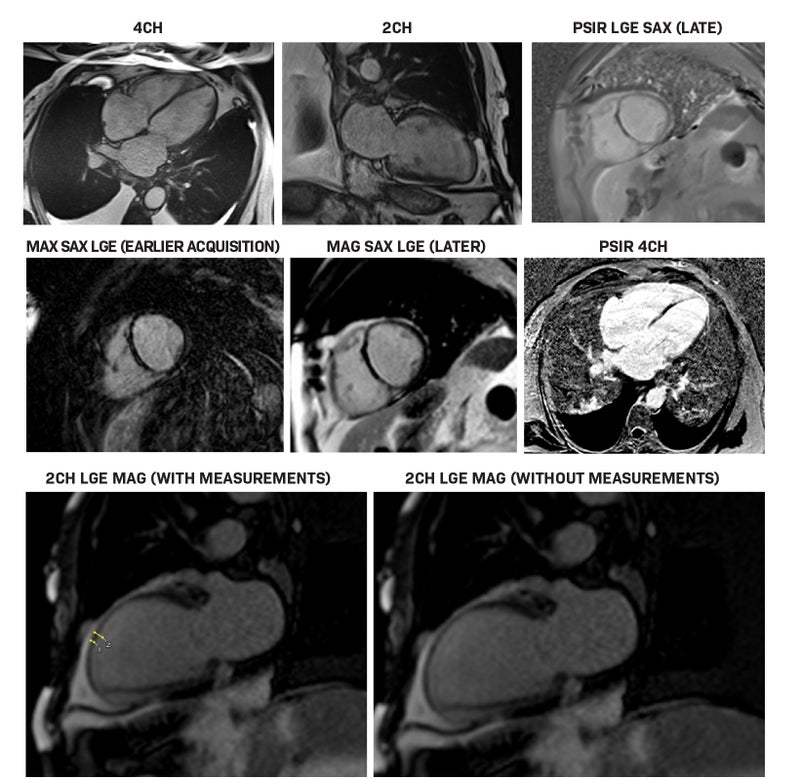
The cardiac MRI revealed globally reduced motion with akinesia of the basal to mid septum and anterior wall, apical segments, and apex. Late gadolinium enhancement (LGE) involving subendocardial basal to apical septum, along with evidence of microvascular obstruction in the rest of the septal myocardium, findings consistent with non-viable myocardium, were appreciated. However, there was subendocardial LGE involving the mid to apical anterior wall with 50% of the wall thickness in the mid anterior wall and 50% of wall thickness in the apical anterior wall, consistent with subendocardial infarction and ischemic cardiomyopathy, but with viable tissue.
The patient was deemed a nonsurgical candidate following evaluation for cardiothoracic surgery. For concerns of acute coronary syndrome, the patient underwent intravascular ultrasonographic guided complex percutaneous intervention with rotational atherectomy and bifurcation stenting of the left circumflex and left anterior descending artery. Cardiac MRI demonstrated with LGE imaging a moderate degree of viability despite substantial myocardial asynergy affording an opportunity for a high-risk intervention. Confirming the cardiac MRI with a subsequent echocardiogram revealed LVEF had improved to 35%, particularly in the anterolateral left anterior descending territory.
Case 4: A Young Woman With Hypereosinophilic Syndrome
We have also used cardiac MRI to diagnose hypereosinophilic syndrome with cardiac involvement. Recently, we saw a female patient in her thirties with a past medical history significant for primary hypertension and hyperlipidemia, and a recent cesarean section, with worsening dyspnea on exertion and orthopnea for one week. On presentation, the patient was tachypneic with sinus tachycardia, elevated blood pressure (150/107 mmHg), and bilateral basilar crackles on pulmonary auscultation. The initial workup, which included a complete blood count, comprehensive metabolic panel, troponin, arterial blood gas, and respiratory pathogen panel, was unremarkable. Brain natriuretic peptide was elevated at 765 (normal, ≤100 pg/mL). A chest x-ray revealed prominent interstitial markings suspicious for fluid overload. A computed tomography scan of the chest with contrast was negative for pulmonary embolism. An echocardiography revealed normal left ventricular size and systolic function. It also revealed endomyocardial thickening of the apical segments and the entire lateral wall, sparing the valves. Testing for Chagas disease was negative. The patient underwent an endomyocardial biopsy, which showed mild myocyte hypertrophy with focally mild vacuolization in the myocytes without inflammatory, fibrotic, or viral cytopathic changes. A cardiac MRI, performed with 6.7 mL of gadopiclenol, revealed a normal left ventricle with mildly decreased systolic function and akinesis of mid inferior, apical anterior, apical septal, apical inferior, and apical lateral walls, as well as the apex (Figure 4).
A female patient in her thirties presenting with worsening dyspnea on exertion and orthopnea for one week. Cardiac MRI (enhanced with 6.7 mL gadopiclenol) led to diagnosis of organ-restricted hyper-eosinophilic syndrome with cardiac involvement without eosinophilic myocarditis. Abbreviations: 2CH, 2 chamber view; 4CH, 4 chamber view; LGE, late gadolinium enhancement; MAG, magnitude; PSIR, phase sensitive inversion recovery; SAX, short axis; TI, inversion time.
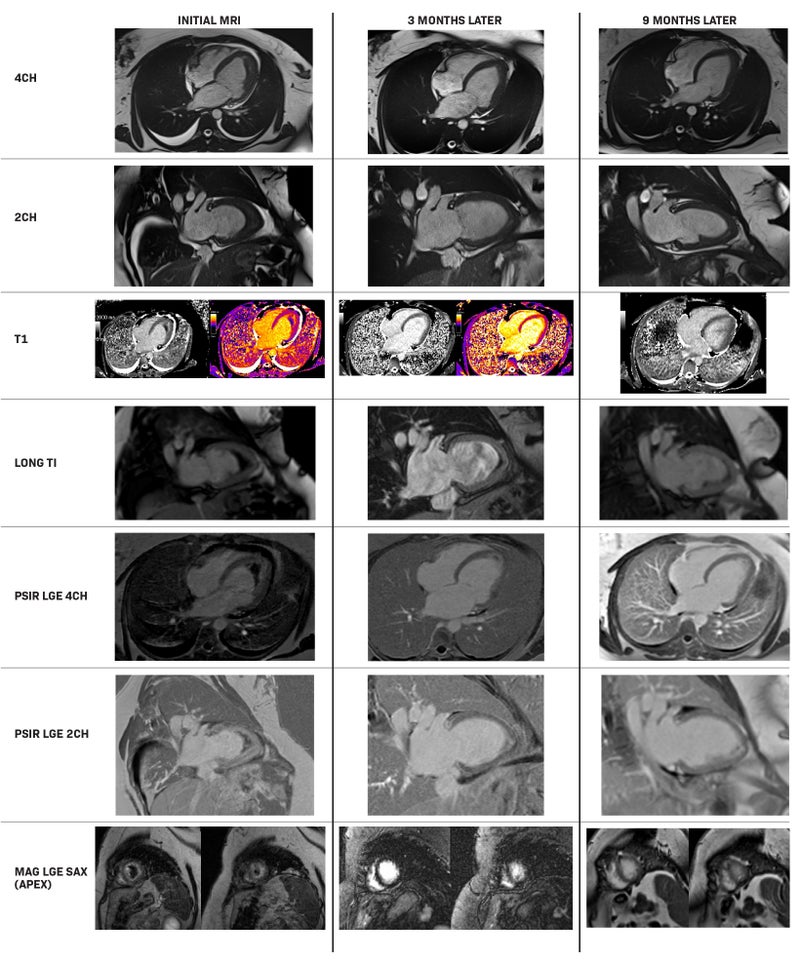
Tissue parametrics demonstrated mildly elevated native T1 time and ECV. There was mid-myocardial LGE in the basal anteroseptal wall, suggesting a myocardial scar from nonspecific fibrosis. A laminar left ventricular apical thrombus measured 18 mm x 51 mm. First-pass perfusion showed a lack of perfusion in the left ventricular thrombus area, a classic ‘Double V’ sign of eosinophilic (Loeffler’s) myocarditis. The patient was diagnosed with organ-restricted hyper-eosinophilic syndrome with cardiac involvement but without biopsy-proven eosinophilic myocarditis, yet with cardiac MRI-pathognomonic Loeffler’s myocarditis. She was discharged home on steroid therapy with guideline-directed medical therapy. The patient underwent a repeat cardiac MRI 6 months later, which revealed a fixed left ventricular thrombus, improvement in size with mid myocardial LGE in the basal interventricular septum, suggesting myocardial scar from nonspecific fibrosis.
Comprehensive genetic testing for 82 genes was negative. A further repeat cardiac MRI at six months revealed subtle LGE in the apical inferior sub-endocardium, with native T1 and ECV mildly elevated; however, T2 time was normal, indicating no evidence of acute inflammation. A very small residual apical thrombus was present, likely entangled in chordae tendinea. The use of gadolinium to confirm the diagnosis and initiate therapeutics was instrumental in this biopsy-negative case under the assumption that the biopsy(s) missed the area of active inflammation as the approach was confined to the right ventricular septum.
Implementation of Gadopiclenol
Historically, many gadolinium-enhanced cardiac MRI techniques were established using higher than recommended body weight dosing (ie, double or one and a half times the standard dose or rarely triple dosing).40,41 This dosing was thought to be necessary to capture pathologies that require more precise differentiation between normal and abnormal structures. With the introduction of gadopiclenol, MR imaging professionals, initially expressed concern that the 0.05 mmol/kg dose could compromise diagnostic quality due to the reduced contrast volume delivered.
In our practice, we successfully transitioned to gadopiclenol for cardiac MRI protocols. The process began with gaining a better understanding of its capabilities at the lower gadolinium dose, and how it could address imaging needs without sacrificing patient safety. After a successful product evaluation period and staff education, we obtained the necessary administrative approvals and updated our cardiac MRI contrast-enhanced protocols. During our evaluation period, we also noted that the approved weight- based dosing of gadopiclenol at 0.05 mmol/kg provided adequate image quality without the need to adjust the saline chaser
post-gadopiclenol infusion. As a result, we have not adjusted the saline chaser across all gadopiclenol-enhanced cardiac MRI scans. Specifically with stress perfusion, we utilize a dose of 0.025 mmol/kg for rest perfusion followed by another 0.025 mmol/kg for stress perfusion. Many times, LGE for viability is indicated, and so we employ an additional 0.025 mmol/kg dose immediately following the stress perfusion. Some centers may prefer only to use stress perfusion imaging and, if normal, eliminate rest perfusion imaging. Alternatively, other centers may utilize stress imaging followed automatically by rest imaging. We prefer to incorporate rest imaging regardless of the clinical findings on stress imaging as a check on the accuracy of the stress findings, as well as to verify the study findings.
Communication and Collaboration
Effective communication and shared knowledge among our multidisciplinary teams are the keys to our success with gadopiclenol use in cardiac MRI. As cardiologists, we enjoy a dynamic working relationship with our radiologists, owing to the fact that our expertise in cardiovascular anatomy and function has been pivotal in educating both radiologists and MRI technologists. This collaboration has helped ensure accurate image acquisition and the identification of abnormalities that help inform clinical decision-making. Therefore, it is recommended that those performing cardiac MRI have a deep understanding of cardiac anatomy, pathology, and physiology in order to elevate patient care.
Notably, MRI technologists play a critical role in achieving a diagnostic cardiac MRI scan. Their advanced technical skills and understanding of cardiac anatomy for cardiac imaging allows them to adapt and think critically in our dynamic environment, thus assisting both radiologists and cardiologists in delivering optimal imaging that impacts patient care. Close collaboration with our cardiologists has augmented the MRI technologists’ training; thus, we have found that a close partnership between the cardiologists and the MRI technologists ensures a diagnostic cardiac MRI examination. When feasible, we recommend that a cardiologist join the MRI technologist during scanning to achieve optimal images and collaborate with the radiologist to support exam interpretation. This collaborative environment aids in a better understanding of each patient’s imaging needs and supports the acquisition of high-quality images that aid clinical diagnosis.
Summary
GBCAs are powerful tools that can improve the diagnostic utility of cardiac MRI examinations through accurate diagnosis and careful disease monitoring, as well as informed treatment planning. The potential risks of GBCAs have led to the development of gadopiclenol, an agent with the highest relaxivity commercially available and high kinetic stability that enables lower gadolinium dosing without sacrificing image quality. Especially for complex cardiac cases, these attributes solidify the value that an agent such as gadopiclenol adds to the cardiac MR physician’s armamentarium. As demonstrated in clinical studies, a 0.05 mmol/kg dose of gadopiclenol provides improved contrast enhancement with high diagnostic accuracy and efficacy compared with a 0.1 mmol/kg dose of standard GBCA. As institutions evolve to adopt gadopiclenol, a staged approach to implementation and multidisciplinary collaboration can enhance diagnostic accuracy and ultimately improve cardiovascular care.
References
- Pfeiffer MP, Biederman RW. Cardiac MRI: a general overview with emphasis on current use and indications. Med Clin North Am. 2015;99(4):849-861.
- Bandettini WP, Arai AE. Advances in clinical applications of cardiovascular magnetic resonance imaging. Heart. 2008;94(11):1485-1495.
- West AM, Kramer CM. Comprehensive cardiac magnetic resonance imaging. J Invasive Cardiol. 2009;21(7):339-345.
- Gajjar K, Kashyap K, Badlani J, Williams RB, Biederman RWW. A review of the pivotal role of cardiac MRI in mitral valve regurgitation. Echocardiography. 2021;38(1):128-141.
- Reddy ST, Shah M, Doyle M, et al. Evaluation of cardiac valvular regurgitant lesions by cardiac MRI sequences: comparison of a four-valve semi-quantitative versus quantitative approach. J Heart Valve Dis. 2013;22(4):491-499.
- Uhlig J, Al-Bourini O, Salgado R, et al. Gadolinium-based contrast agents for cardiac MRI: use of linear and macrocyclic agents wih associated safety profile from 154 779 European patients. Radiol Cardiothorac Imaging. 2020;2(5):e200102.
- American College of Radiology (ACR) Committee on Drugs and Contrast Media. ACR Manual on Contrast Media, 2024. https://www.acr.org/-/media/ACR/Files/ Clinical-Resources/Contrast_Media.pdf. Accessed July 27, 2024.
- VUEWAY® (gadopiclenol) solution for injection, 485.1 mg/mL. Full Prescribing Information and Medication Guide. Bracco Diagnostics. Princeton, NJ; March 2025.
- Elucirem™ (gadopiclenol) injection. Full Prescribing Information. Princeton, NJ: Guerbet LLC.; March 2025.
- Kanal E, Maravilla K, Rowley HA. Gadolinium contrast agents for CNS imaging: current concepts and clinical evidence. AJNR Am J Neuroradiol. 2014;35(12):2215-2226.
- Ipek R, Holland J, Cramer M, Rider O. CMR to characterize myocardial structure and function in heart failure with preserved left ventricular ejection fraction. Eur Heart J Cardiovasc Imaging. 2024;25(11):1491-1504.
- Plehn JF, Biederman RWW. Diffuse myocardial fibrosis in dilated cardiomyopathy: risk marker, risk factor, or does it matter? JACC Cardiovasc Imaging. 2022;15(4):591-593.
- Rathi VK, Czajka AT, Thompson DV, et al. Can cardiovascular MRI be used to more definitively characterize cardiac masses initially identified using echocar diography?. Echocardiography. 2018;35(5):735-742.
- Ibrahim T, Nekolla SG, Schreiber K, et al. Assessment of coronary flow reserve: comparison between contrast-enhanced magnetic resonance imaging and positron emission tomography. J Am Coll Cardiol. 2002;39(5):864-870.
- Schwitter J, Nanz D, Kneifel S, et al. Assessment of myocardial perfusion in coronary artery disease by magnetic resonance: a comparison with positron emission tomography and coronary angiography. Circulation. 2001;103(18):2230-2235.
- Robic C, Port M, Rousseaux O, et al. Physicochemical and pharmacokinetic profiles of gadopiclenol: a new macrocyclic gadolinium chelate with high T1 relaxivity. Invest Radiol. 2019;54(8):475-484.
- Rohrer M, Bauer H, Mintorovitch J, Requardt M, Weinmann HJ. Comparison of magnetic properties of MRI contrast media solutions at different magnetic field strengths. Invest Radiol. 2005;40(11):715-724.
- ProHance® (Gadoteridol) Injection, 279.3 mg/mL. Full Prescribing Information and Medication Guide Bracco Diagnostics. Princeton, NJ; March 2025.
- Gadavist® (gadobutrol) injection. Full Prescribing Information. Whippany, NJ: Bayer Healthcare Pharmaceuticals; March 2025.
- Dotarem® (gadoterate meglumine) injection. Full Prescribing Information. Princeton, NJ: Guerbet LLC.; March 2025.
- Clariscan™ (gadoterate meglumine) injection. Full Prescribing Information. Marlborough, MA: GE Healthcare Inc.; September 2024.
- MultiHance® (gadobenate dimeglumine) injection, 529 mg/mL. Full Prescribing Information and Medication Guide. Bracco Diagnostics. Princeton, NJ; March 2025.
- Eovist® (gadoxetate disodium) injection. Full Prescribing Information. Whippany, NJ: Bayer HealthCare Pharmaceuticals; March 2025.
- Maravilla KR, Maldjian JA, Schmalfuss IM, et al. Contrast enhancement of central nervous system lesions: multicenter intraindividual crossover comparative study of two MR contrast agents. Radiology. 2006;240(2):389-400.
- Rowley HA, Scialfa G, Gao PY, et al. Contrast-enhanced MR imaging of brain lesions: a large-scale intraindividual crossover comparison of gadobenate dimeglumine versus gadodiamide. AJNR Am J Neuroradiol. 2008;29(9):1684-1691.
- Seidl Z, Vymazal J, Mechl M, et al. Does higher gadolinium concentration play a role in the morphologic assessment of brain tumors? Results of a multicenter intraindividual crossover comparison of gadobutrol versus gadobenate dimeglumine (the MERIT Study). AJNR Am J Neuroradiol. 2012;33(6):1050-1058.
- Vaneckova M, Herman M, Smith MP, et al. The benefits of high relaxivity for brain tumor imaging: results of a multicenter intraindividual crossover comparison of gadobenate dimeglumine with gadoterate meglumine (The BENEFIT Study). AJNR Am J Neuroradiol. 2015;36(9):1589-1598.
- Martincich L, Faivre-Pierret M, Zechmann CM, et al. Multicenter, double-blind, randomized, intraindividual crossover comparison of gadobenate dimeglumine and gadopentetate dimeglumine for Breast MR imaging (DETECT Trial). Radiology. 2011;258(2):396-408.
- Pediconi F, Kubik-Huch R, Chilla B, Schwenke C, Kinkel K. Intra-individual randomised comparison of gadobutrol 1.0 M versus gadobenate dimeglumine 0.5 M in patients scheduled for preoperative breast MRI. Eur Radiol. 2013;23(1):84-92. Published correction appears in Eur Radiol. 2013;23(8):2100.
- Kramer JH, Arnoldi E, François CJ, et al. Dynamic and static magnetic resonance angiography of the supra-aortic vessels at 3.0 T: intraindividual comparison of gadobutrol, gadobenate dimeglumine, and gadoterate meglumine at equimolar dose. Invest Radiol. 2013;48(3):121-128.
- Loevner LA, Kolumban B, Hutóczki G, et al. Efficacy and safety of gadopiclenol for contrast-enhanced MRI of the central nervous system: the PICTURE randomized clinical trial. Invest Radiol. 2023;58(5):307-313.
- Kuhl C, Csőszi T, Piskorski W, Miszalski T, Lee JM, Otto PM. Efficacy and safety of half-dose gadopiclenol versus full-dose gadobutrol for contrast-enhanced body MRI. Radiology. 2023;308(1):e222612.
- Idée JM, Port M, Robic C, Medina C, Sabatou M, Corot C. Role of thermodynamic and kinetic parameters in gadolinium chelate stability. J Magn Reson Imaging. 2009;30(6):1249-1258.
- McDonald RJ, Levine D, Weinreb J, et al. Gadolinium retention: a research roadmap from the 2018 NIH/ACR/RSNA workshop on gadolinium chelates. Radiology. 2018;289(2):517-534.
- Fretellier N, Rasschaert M, Bocanegra J, et al. Safety and gadolinium distribution of the new high-relaxivity gadolinium chelate gadopiclenol in a rat model of severe renal failure. Invest Radiol. 2021;56(12):826-836.
- Funke SKI, Factor C, Rasschaert M, et al. Long-term gadolinium retention in the healthy rat brain: comparison between gadopiclenol, gadobutrol, and gadodiamide. Radiology. 2022;305(1):179-189.
- Rasschaert M, Couloumy E, Renard E, et al. Reduced Gd exposure over 5 months after a single human equivalent dose of gadopiclenol as compared to gadobutrol in healthy rats. Neuroradiology. 2023;65(Suppl):S580(1-P37).
- Spinazzi A, Lancelot E, Vitali L, et al. Safety of gadopiclenol after its first year of clinical use. Invest Radiol. Published online November 21, 2024.
- Russo AM, Desai MY, Do MM, et al. ACC/AHA/ASE/HFSA/HRS/SCAI/SCCT/SCMR 2025 appropriate use criteria for implantable cardioverter-defibrillators, cardiac resynchronization therapy, and pacing. J Am Coll Cardiol. 2025;85(11):1213-1285.
- Kramer CM, Barkhausen J, Bucciarelli-Ducci C, Flamm SD, Kim RJ, Nagel E. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson. 2020;22(1):17.
- Paiman EHM, Lamb HJ. When should we use contrast material in cardiac MRI? J Magn Reson Imaging. 2017;46(6):1551-1572.